egg donors

A Complete Guide to Understanding Your Egg Donor’s Genetic Testing Results
Choosing an egg donor? Understanding their genetic testing summary is key. Here’s what you need to know about carrier status, compatibility, and making confident, informed choices.
Choosing an egg donor is one of the most meaningful steps in building your family through donor egg IVF. Among the many important factors to consider (like personal background, physical traits, and education), one of the most medically relevant is your egg donor’s genetic testing summary.
Understanding your donor’s genetic profile helps ensure genetic compatibility between the donor and the sperm source, which reduces the chance of passing on inherited conditions. Whether you’re pursuing a frozen or fresh egg donation, interpreting these results can feel overwhelming at first. But with the right guidance, you can make an informed, confident choice.
In this guide, we’ll help you understand:
- What’s included in an egg donor’s genetic testing summary
- The importance of genetic compatibility in egg donation
- How to interpret terms like “carrier,” “variant of uncertain significance,” and more
- What to do if your donor and sperm source aren’t genetically compatible
- How a genetic counselor can support your journey
At Cofertility, we prioritize transparency and genetic safety. For all fresh and frozen matches, we provide a genetic testing summary. However, during a fresh donation, this happens after the match. All of our donors complete the Fulgent Beacon Expanded Carrier Screening panel which tests for 427 conditions. If you have already completed a different panel, follow-up testing may be recommended for you or your donor. Recommendations for additional testing should be discussed with your reproductive endocrinologist and/or a genetic counselor.
No matter how you go about it, genetic testing is a big deal, and it’s critical that you fully understand the results for both the egg donor and sperm source. Read on so that you can feel fully informed and confident as you move forward through the donation process.
Why genetic testing matters in donor egg IVF
Genetic testing plays a vital role in identifying recessive and X-linked conditions that may otherwise go unnoticed. Most people are carriers of at least one genetic condition, even without any symptoms. If both the donor and the sperm source are carriers for the same condition, the risk of having a child affected by that condition increases significantly.
Understanding inheritance patterns
Autosomal recessive inheritance: Both biological contributors must be carriers of the same gene mutation for the child to be at risk. If only one is a carrier, the child is usually unaffected.
X-linked inheritance: This type affects conditions linked to genes on the X chromosome. If a donor carries an X-linked condition and the child is biologically male, he may be at risk.
Think of genes like recipe cards. A mutation is like a typo on the card. If both sets of recipe cards (from egg and sperm) have the same typo, the dish — or baby — might turn out differently than expected.
In some cases, this could also result in an increased risk of miscarriage or pregnancy loss, especially if the condition is severe and incompatible with life. Some affected embryos may fail to implant or stop developing early on.
Learn more about carrier screening and inheritance here.
How to interpret genetic testing results
Your egg donor’s genetic profile may include one or more of the following:
1. Chromosome analysis (karyotype)
A karyotype looks at the structure and number of chromosomes. It can detect large-scale abnormalities such as translocations, deletions, or extra chromosomes (e.g., Turner syndrome or balanced translocations). These abnormalities can affect fertility or the health of the resulting embryo.
2. Hemoglobin evaluation
This test screens for conditions like sickle cell disease or thalassemia, which are more common in certain ethnic groups. It assesses the type and quantity of hemoglobin in the blood.
3. Carrier screening
The most extensive and detailed part of the genetic testing summary. It examines hundreds of genes associated with recessive and X-linked conditions.
At Cofertility, whenever possible, we utilize the Fulgent Beacon 427 panel, which tests for over 400 clinically relevant genes, including cystic fibrosis, Tay-Sachs disease, and spinal muscular atrophy (SMA).
Interpreting an egg donor’s carrier screening results
Here are some terms that you may find in your donor’s genetic testing summary:
- “Carrier”: The donor carries one mutated copy of a gene for a recessive or X-linked condition but is not affected. This is common and doesn’t automatically disqualify the donor.
- “Variant of Uncertain Significance (VUS)”: A genetic variant was found, but it’s unclear whether it causes disease. These are not typically considered a match-breaking finding.
- “Reproductive risk”: This refers to the chance that a child could inherit a condition based on both donor and sperm source being carriers of the same gene.
One important note: different labs use different naming conventions and may include different genes in their panels. That’s why it’s crucial to match the donor and sperm source panels, or at least confirm both were tested for the same conditions.
Clinics often have preferred testing labs (like Fulgent, Natera, or Sema4). If you or your donor switch clinics mid-process, your new clinic may accept prior testing as long as results cover the same conditions.
What if the egg donor and sperm source are not a genetic match?
Even with rare mutations, this is possible. When it does, there are several options:
- Genetic counseling: Speak with a licensed counselor to understand your risks and whether additional testing is warranted.
- Donor re-selection: If the risk is deemed too high, choosing a new donor is always an option.
- PGT-M testing: In some cases, preimplantation genetic testing for monogenic disorders (PGT-M) may be used to select embryos free of the condition.
The role of a genetic counselor
A genetic counselor is a trained healthcare professional who can help interpret complex genetic reports and explain inheritance risks in plain language. They’ll also help you coordinate follow-up testing or next steps and support your emotional well-being throughout the process.
In other words? Genetic counselors are a godsend for average patients who want to clearly understand genetic testing summaries. At Cofertility, we encourage all intended parents to connect with a genetic counselor, especially when navigating genetic compatibility throughout the egg donation process.
FAQs about egg donor genetic testing
What if my donor is a carrier?
That’s common, and not necessarily a concern. What matters is whether the sperm source is a carrier for the same condition.
Can I request additional testing for the donor?
Yes. If your clinic or doctor recommends more targeted screening, it can often be arranged through your Cofertility Member Advocate.
Do I need to be tested too?
If you are using your own sperm or a known sperm source, yes. Your clinic may have already tested you. If not, you can request it as part of the match process.
Why are results from different labs hard to compare?
Each lab uses slightly different panels and reporting methods. That’s why matching the same or equivalent panel is essential to properly assess reproductive risk.
Making informed choices with confidence
Your egg donor’s genetic testing summary is a critical tool in making a safe and informed decision about your path to parenthood. With the right information, plus the support of your clinic and genetic counselor, you can interpret your donor’s results confidently and understand how they align with your family-building goals.
Cofertility is here to support you every step of the way. If you have questions about a donor’s genetic testing summary or want to ensure compatibility, reach out to our team. We’ll help guide you through the process with compassion and clarity.

5 Things No One Tells You About Using Donor Eggs
Using donor eggs to build your family can stir up more than just excitement—it may bring grief, identity questions, and unexpected moments of reflection. Here are five emotional truths no one really talks about.
Becoming a parent through egg donation is an extraordinary journey, one filled with hope, love, and often, unexpected emotional complexity. As a licensed clinical psychologist specializing in fertility, I have spent nearly two decades walking alongside individuals and couples as they navigate third-party reproduction. My work focuses on the emotional layers that often go unspoken: grief, identity, and bonding.
In this article, I’ll share five things no one really tells you about using donor eggs, truths I have learned not just through clinical training, but through the voices and stories of the many families I have supported. These insights are here to help you feel more prepared, less alone, and more confident in the deeply personal path you are on.
1. It’s ok to grieve your genetic connection—even if you're excited
It is completely normal to feel a complex mix of emotions when using donor eggs. You may feel immense gratitude and excitement about becoming a parent, yet still grieve the lack of a genetic connection. Remember that these two feelings can coexist. Acknowledging your grief does not diminish your joy. In fact, giving yourself permission to process these emotions is an act of self-care.
Tip: Consider speaking with a therapist who specializes in fertility or joining a support group for people using donor eggs; sharing your experience with others who understand can help you process these feelings so you don’t feel alone in these feelings.
2. You may start seeing your donor in your child
As your child grows, you might notice features, gestures, or ways of thinking that feel... not quite yours. Perhaps it is the shape of their nose, their sense of humor, or how they tilt their head when they think. These traits may resemble something you saw in a photo or read in a profile. This can be deeply moving, but also disorienting.
Rather than trying to “fix” uncomfortable emotions, we can practice willingness by making space for those uncomfortable emotions without judgment. When a moment of recognition arises and brings a pang of unfamiliarity or longing, it can help to pause and notice: What value is this emotion pointing to? Often, these feelings reflect your desire to feel fully connected.
According to the American Society for Reproductive Medicine (ASRM), intended parents should be made aware that genetic contributors may remain “psychologically present” over time, especially in known/direct arrangements. That presence does not need to be feared or avoided. Instead, it can become part of your child’s story.
Tip: Being mentally prepared for the donor’s ongoing presence in subtle ways can help ease unexpected emotions. Try naming what comes up: “I feel a little sad that I don’t see myself in this moment, and I also feel wonder at who they are becoming.”
3. Openness from day one matters more than you think
When it comes to talking to your child about their beginnings, early and honest conversations aren’t just recommended—they are profoundly protective. Research and guidance from ASRM emphasize that children benefit from being told about their donor origins at a young age, using simple, developmentally appropriate language.
Leaning into these conversations, even when they feel vulnerable or uncertain, is an act of living in alignment with your parenting values: love, openness, and trust. Practicing psychological flexibility means allowing your own discomfort (if it arises) to be present, without letting it dictate your actions.
Tip: Look for children’s books that explain donor conception in age-appropriate language. These can help make the conversation feel natural.
4. Genetic health information is a lifelong need
Choosing an egg donor doesn’t end with matching profiles. As your child grows, so does their need for ongoing access to genetic health information. Pediatricians and specialists may ask for extended family history if medical concerns arise. That’s why selecting a donor through a program that allows for future medical updates, or even open communication, can be invaluable.
Consider: Ask your egg donation program how they handle long-term updates to the donor’s medical history.
5. You’ll form a bond that transcends genetics
It is a common fear: What if I don’t feel connected to my child? For many intended parents using donor eggs, the absence of a genetic link stirs quiet doubts about bonding. But over and over, families share that the love they experience is not only real, it is often deeper than they could have imagined. Connection isn’t dictated by DNA; it is cultivated in the everyday rhythms of parenting.
Our minds often generate fear-based stories, especially when we’re stepping into the unknown. These thoughts “What if I don’t feel like their real parent?” don’t need to be judged or pushed away. Instead, we can notice them with compassion, then return to the values that led us here: the desire to nurture, protect, and love a child.
Bonding doesn’t happen all at once. It forms in the small, repeated acts of care—midnight feedings, diaper changes, and warm cuddles. And research continues to affirm that the quality of parent-child relationships has little to do with genetic ties and everything to do with presence, attunement, and emotional responsiveness.
Reassurance: Love is built in daily moments, not shared DNA.
Using donor eggs to build your family is both a medical decision and a deeply human one. It’s okay to feel a mix of joy, grief, uncertainty, and love as you move forward. The most important thing is that you’re showing up with intention, care, and an open heart. However your child comes into your life, your love—the kind built in daily, imperfect, beautiful moments—is what truly defines family.
Read more:

How to Use SART Data to Evaluate Fertility Clinics for Donor Egg IVF
Wondering how to evaluate fertility clinics for donor egg IVF? The SART database is a helpful place to start—but only if you know how to read between the lines. Here’s what to look for (and what to question).
When you’re pursuing egg donation to build your family, choosing the right fertility clinic can feel overwhelming. Everyone wants the best outcomes possible and while there’s no perfect formula for picking a clinic, the Society for Assisted Reproductive Technology (SART) database is one tool we have to evaluate IVF clinics.
SART collects detailed outcome data from hundreds of clinics across the U.S., reporting on everything from the number of cycles completed to live birth rates by patient age and treatment type. But understanding what the numbers mean and how to apply them to your unique family-building plans takes a bit of interpretation. For example, a clinic that reports higher live birth rates might simply be selecting patients with fewer fertility barriers, while another with more modest numbers could be working with harder-to-treat cases, including people with diminished ovarian reserve or complex medical histories.
This article walks through how to make sense of the SART Clinic Report, what success rates do (and don’t) tell you, and which filters are most relevant when you’re planning to use donor eggs. We’ll also cover red flags to watch for and other questions you should be asking alongside the data.
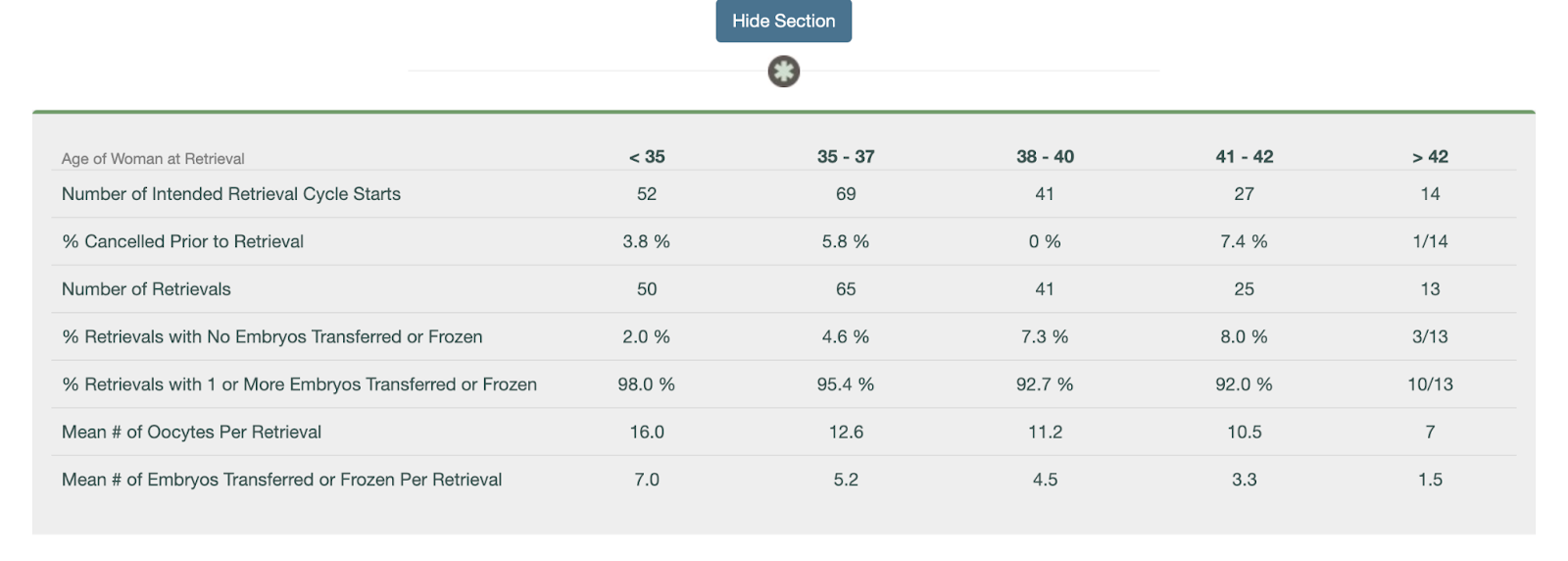
What SART data can tell you—and what it can’t
SART data is one of the most widely used sources for clinic success rates, as it reflects real outcomes, including pregnancies and live births after IVF. But it’s not a perfect apples-to-apples comparison tool. For starters, SART data is self-reported by clinics and reviewed for consistency, but not independently audited in full.
SART data also lags about two years behind, since it only includes cycles that have had time to result in a live birth. If you’re working with a newer clinic, they could be tracking and reporting outcomes to SART but just may not be reflected in the dataset quite yet.
The data is reported by cycle start, which includes any patient who initiated an IVF cycle, even if they didn’t proceed to egg retrieval or embryo transfer. That means reported live birth rates may include a denominator of patients who never got far enough for the treatment to have a real chance of success. Some clinics work hard to include every patient in their reported data; others may be more selective about who they treat, which can make their success rates appear higher.
Still, if you understand what you’re looking at, SART data can provide real insight, especially when you use filters and hone in on metrics that apply to your situation.
Looking up donor egg cycles in the SART report
To start, you can look up an IVF clinic by name or location here. If a clinic has multiple locations: they may have profiles associated with every location or they may only have profiles associated with their primary labs. The search functionality is also a bit sensitive; if you’re not locating a clinic by name, try searching by city or state.
When viewing a clinic’s report, you’ll see multiple sections, each focusing on different treatment types: cycles using a patient’s own eggs, cycles using donor eggs, and cycles using donated embryos. For intended parents working with an egg donor and possibly a gestational carrier, the donor egg data is most relevant.
Here’s what you’ll see in the donor egg section:
- Fresh donor egg cycles: These are cycles that involve using fresh donor eggs and a fresh embryo transfer.
- Frozen donor egg cycles: These are cycles that involve using frozen donor eggs and a fresh embryo transfer.
- Donor egg thawed embryos: These are cycles using frozen embryos (thawed before transfer) that were made with either fresh or frozen donor eggs.
- Donated embryos: These involve embryo transfers using embryos that were originally created by another individual or couple. These are all frozen embryo transfers.
Each of these comes with its own success rates, reported by age and often by the number of embryos transferred.
Understand the difference between a Fresh vs Frozen Embryo Transfer.
How to interpret success rates in the SART report
Once you’ve identified the donor egg section of a clinic’s SART report, you can start digging into the numbers. While the report doesn’t include every metric (like implantation rate), it does offer helpful data points to understand how often donor egg cycles result in live births—and how experienced the clinic is with this kind of care.
Here’s how to use the data:
- Look at the total number of embryo transfer procedures. This tells you how many donor egg transfers the clinic performed, which can give you a sense of their experience. A higher number means the clinic is regularly working with donor egg IVF families—an important signal if you’re pursuing this type of treatment.
- Check how many of those transfers resulted in live births. If there are fewer than 10 cycle starts in a category, live births are provided as a fraction. If there are 11 or more cycles, it’s provided as a percentage. While this isn’t a perfect metric, it offers a practical look at how effective the clinic is once a transfer occurs.
- Review singleton vs. multiple birth rates. A high singleton rate suggests the clinic emphasizes single embryo transfer (eSET), which is generally safer for both the carrier and the baby. High twin rates may boost reported pregnancy success but come with higher medical risks.
- If you’re using a gestational carrier (GC), ask the clinic for donor egg + GC outcomes. SART doesn’t break this out, but clinics should be able to provide this data. These cycles tend to be highly optimized and can reflect the clinic’s best-case outcomes.
While the SART report doesn’t show everything, it provides a meaningful snapshot of how well a clinic performs with donor egg cycles and how often they’re managing them. Combine this data with direct questions to the clinic to get a fuller picture of what you can expect.
Consider volume, but don’t assume more is always better
SART data shows how many cycles a clinic performs in a given year. Higher volume can indicate more experience and familiarity with a wide range of cases, but that doesn’t mean bigger is always better. A massive clinic might have shorter visit times, less personalized attention, or limited communication with physicians. Conversely, smaller clinics may offer more personalized care but might not have the same technological resources or lab investment.
Ask yourself what matters more to you: personalized attention and consistency, or access to a busy, highly specialized team? There’s no right answer—just what fits your preferences.
Don’t ignore what’s missing
Some clinics don’t report data to SART at all. While SART participation is voluntary, transparency should be a baseline expectation. If a clinic doesn’t report, ask why. It might be a red flag, or it might be an early-stage clinic without a full year of data yet.
It’s also worth noting that SART doesn’t report standalone success rates for thawed eggs (only fresh embryo transfers). So if you’re using frozen donor eggs—or if you’re planning to freeze embryos now and transfer later—those specific success rates won’t be visible. In those cases, ask the clinic directly about their outcomes from egg thaw cycles and embryo transfers using frozen material.
Be cautious about over-interpreting live birth per cycle
Clinics are incentivized to make their live birth per retrieval cycle look high, which can lead to some concerning practices like encouraging patients to transfer an embryo right away instead of banking multiple embryos for future family-building, or discouraging care for “poor responders” who may require multiple retrievals. These choices may boost reported rates but aren’t always in a patient’s best interest.
For intended parents hoping to have more than one child using the same donor, it may be smarter to focus on embryo banking before any transfer. But this approach - although strategic - can negatively impact the clinic’s live birth per cycle numbers. That’s why it's important to ask how your clinic approaches embryo banking and cumulative success planning.
Other questions to ask beyond the numbers
While SART data is valuable, it’s only one part of the clinic evaluation process. Consider also asking:
- What’s the average number of embryos your clinic transfers per cycle?
- How do you support intended parents using donor eggs or gestational carriers?
- What’s the experience like for people working with donor eggs?
You might also want to explore patient reviews on sites like FertilityIQ or attend a clinic info session to get a better feel for their values and communication style.
Bottom line
SART data can be a powerful tool when selecting a fertility clinic if you know how to use it wisely. Focus on donor egg cycles, apply relevant filters, and pay close attention to metrics like number of transfers, singleton birth rate, and outcomes per embryo transfer. Use the data to inform your questions, not as the only measure of quality.
Look for transparency, clarity, and a clinic that welcomes your questions. The right data can support your decision, but trust and care matter just as much.
If you work with Cofertility, we can help connect you with one of our many clinic partners.
Read more:

Choosing an Egg Donor: The Role of Biomarkers
Choosing the right egg donor involves more than just age. Learn how fertility doctors use AMH, AFC, and age together to predict egg yield and guide your family-building decisions.
If you're pursuing egg donation to build your family, you’ve probably heard that age matters. However, when it comes to the number of eggs a donor might produce in a single cycle, age is only part of the picture. Fertility doctors use a combination of biological indicators called ovarian reserve markers to get a clearer sense of how a donor is likely to respond to stimulation medication. These markers include AMH (anti-Müllerian hormone), AFC (antral follicle count), and yes, age. Together, they can help predict how many eggs a donor might yield in a given cycle.
Understanding these biomarkers can help you make better decisions: whether that’s about which donor to match with, whether to split a cohort, or whether you may need multiple cycles to meet your family-building goals. This article explains what each of these markers means, how they’re used in donor screening, and what they can (and can’t) tell you about potential outcomes.
Donor AMH: anti-Müllerian hormone
AMH is a hormone released by cells in developing egg follicles. It gives a general sense of a person’s’s ovarian reserve, or the number of eggs they still have. In most people, AMH levels peak in the mid-20s. For intended parents working with an egg donor, a higher AMH level usually suggests the donor has a good chance of responding well to ovarian stimulation, meaning more eggs are retrieved in a single cycle.
That said, there’s a wide range of what’s considered “normal,” and AMH is just one piece of the puzzle. A very high AMH might raise the risk of ovarian hyperstimulation syndrome (OHSS), especially in donors with polycystic ovary syndrome (PCOS). While high AMH may seem appealing at first glance, it still needs to be considered within the broader clinical context. On the other hand, a lower AMH doesn’t necessarily mean a donor isn’t a good candidate, especially if they’re young and have a good antral follicle count.
At Cofertility, an AMH level of at least 2.0 ng/mL is required for our donors. This threshold is based on clinical data suggesting that donors with this level are more likely to have a strong response to fertility medications and produce enough eggs to support both donation and personal use.
AMH is measured through a simple blood test and is often one of the first screening tools used to assess a donor’s fertility potential.
Read more in Does AMH Matter When Choosing an Egg Donor?
Donor AFC: antral follicle count
Antral follicle count is a snapshot of how many follicles are visible on a donor’s ovaries at a particular point in their cycle, usually early in the menstrual cycle, when baseline testing is done. These are the small, fluid-filled sacs that each contain an immature egg. During a stimulation cycle, the follicles grow larger and the eggs inside them mature ,making them available for retrieval.
AFC is measured by transvaginal ultrasound, and it gives a real-time look at the ovaries. The more antral follicles, the higher the potential number of eggs that could be retrieved. In clinical terms, a “normal” AFC is typically somewhere between 10 and 20 follicles (counting both ovaries), but many donors exceed that.
AFC is considered one of the most reliable indicators of ovarian response. While AMH tells you about the pool of follicles available in a more general sense, AFC shows you what’s happening right now. Since AFC is a real-time snapshot of the ovaries, it can fluctuate slightly from month to month, but these variations are typically minor and don’t significantly impact how a donor is expected to respond. For intended parents, a donor with a strong AFC may provide reassurance that the stimulation cycle will likely yield a solid number of mature eggs.
Donor age: still an important piece of the puzzle
You already know age is a factor. But what’s important to understand is that age affects not just the number of eggs a donor may produce, but also the quality of those eggs—specifically, their likelihood of leading to a healthy embryo.
That’s why most egg donation programs set an age range for donors, usually between 21 and 33 years old (we follow these guidelines at Cofertility). While there’s no legal maximum age to become an egg donor, the American Society for Reproductive Medicine (ASRM) recommends that donors be under 34, and most clinics follow that guidance. Our limit accounts for the fact that it can take some time to match with intended parents and complete a cycle, and we want donors to still fall within the recommended age window by the time the cycle takes place.
Within that range, there can still be differences in both quantity and quality of eggs based on things beyond age.
That said, most donors who get medical clearance respond very well to stimulation and produce excellent-quality eggs, whether in their late 20s and early 30s. Age is just one variable, and when combined with the other biomarkers, it helps doctors build a fuller picture of what to expect from a cycle.
How these markers are used together
No single biomarker tells the whole story. Fertility doctors look at AMH, AFC, and age together to estimate a donor’s likely response to ovarian stimulation. This is sometimes called “ovarian reserve testing,” but the goal isn’t just to count eggs. It’s also to plan appropriately for stimulation protocols and optimize outcomes.
For example, if a donor has high AMH and high AFC, they might be expected to produce 20+ eggs in a cycle, and the care team may start with a lower dose of stimulation medications to reduce the risk of overstimulation. If another donor has AMH on the lower end of the normal range and an average AFC, the team may anticipate a more moderate yield (perhaps 10 to 15 eggs) and plan accordingly by using a higher starting dose of medications to optimize their response to treatment.
Limits of prediction
While AMH and AFC are helpful, they’re not crystal balls. A donor with stellar biomarkers could still have a retrieval cycle that yields fewer mature eggs than expected. Likewise, a donor with average numbers might surprise everyone with a strong response.
Biology isn’t always predictable, and cycle outcomes can vary even in the same donor across multiple cycles. That’s why experienced clinics combine biomarker data with close monitoring during the stimulation phase to make adjustments in real time.
It’s also worth noting that the number of eggs retrieved isn’t the only metric that matters. Fertilization rate, embryo development, and success rates with IVF transfer all depend on additional factors,some of which can’t be measured ahead of time.
What this means for you as an intended parent
As you look through donor profiles, you may see some numbers directly—such as AMH or age—or you might get a broader summary from your clinic about the donor’s reproductive potential. It’s a good idea to ask your doctor what these biomarkers might suggest about how many eggs the donor is likely to produce, and how that aligns with your goals.
That said, it’s important to understand that every donor listed has already cleared a rigorous screening process. Fewer than 5% of applicants are accepted into Cofertility’s egg sharing program. If a donor has made it through, it means our medical advisors (who are board-certified reproductive endocrinologists) have reviewed their health, biomarkers, and ovarian reserve, and determined if they’re likely to respond well to treatment.
Within this highly qualified group, small differences in biomarker levels may not translate to big differences in actual outcomes. Rather than fixating on a slightly higher AMH or AFC, it may be more helpful to focus on which donor feels like the right match for your family, whether that’s based on their background, values, personality, or something less tangible that just clicks for you.
The bottom line
AMH, AFC, and age can offer helpful insight into how many eggs a donor may produce and how your doctor will approach their care during the cycle. These biomarkers are useful tools for setting expectations and guiding decisions, but they’re not guarantees.
All egg donation involves some level of uncertainty, even with strong indicators. That’s why programs like Cofertility set high standards up front. This ensures that every donor in the pool has a solid chance of success. Once a donor is approved, the differences between candidates tend to narrow, and the best choice is often the one that feels most aligned with your values and goals—not just the numbers.
Ask questions, gather information, and talk with your care team. But don’t be afraid to trust your gut, too. The right match will meet both the medical criteria and feel like someone who could help you build the family you’ve been hoping for.
Read more:
- Why Egg Donor Age Matters (And Why It Doesn't)
- Does AMH Matter When Choosing an Egg Donor?
- Will My Baby Look Like Me If I Use an Egg Donor?
- Shared vs. Separate Egg Donor Cycles: A Guide for Gay Dads

How Hopeful Gay Dads Decide Whose Sperm to Use
For gay dads growing their families through egg donation, deciding whose sperm to use is deeply personal. This guide breaks down your options, from splitting eggs to leaving parentage unknown and helps you move forward with confidence.
For gay dads growing their families through egg donation and surrogacy, deciding who will contribute sperm is often one of the most meaningful and sensitive decisions in the process. Whether both partners want a biological connection to their child, or just one plans to contribute genetically, there’s no single right way to go about it.
Some couples know right away what feels best. Others spend a lot of time navigating emotional, practical, and medical questions before landing on a plan. And for many, it’s not only about who contributes sperm, but also how. There are multiple ways to approach fertilization, each with its own implications for cost, family dynamics, and personal identity.
In this article, we’ll walk through the most common options for sperm contribution in egg donor cycles for gay dads: using a single sperm source, splitting the eggs, mixing sperm, or choosing to intentionally not know. We’ll also cover what to consider medically and emotionally, and how this choice connects with another big decision: whether to do a shared or separate egg donor cycle (as discussed in this companion guide).
Single sperm source
In this approach, one partner's sperm is used to fertilize all of the donor eggs. It’s the simplest from a medical and logistical standpoint. Some couples choose this route early in the process, while others come to it after weighing various emotional and financial considerations.
Why this works for some couples:
- One partner has a strong preference to be the genetic parent, while the other partner is completely comfortable not contributing sperm.
- A sperm analysis reveals that one partner’s sample has higher quality or fewer risks.
- The couple plans to use the other partner’s sperm for a future child instead of trying to split one egg donor cycle. Or the other partner already has biological children.
This route typically makes embryo creation, storage, and embryo transfer planning more straightforward. It also avoids the risk of uneven embryo numbers between partners, which can come up when splitting a cycle.
But it’s worth talking openly about how this decision feels for both partners. Even when there’s agreement, that doesn’t mean there aren’t emotions to process around roles, fairness, and the relationship each parent will have to the child.
Split insemination
Also known as a “shared cycle,” this option involves dividing the donor eggs between the two partners. Half the eggs are fertilized with one dad’s sperm, and the other half with the other’s. While each partner’s sperm will fertilize the same number of eggs (or close to the same number if there’s an odd number of eggs), this doesn’t mean that there will be the same number of embryos made. That is because each egg is different, each sperm is different, and so there’s some randomness in final outcomes. That being said, in a shared cycle, the goal is two sets of embryos, one per partner.
This option is common among couples who want both dads to be biological parents and are working with one donor cycle to hopefully have two (or more) children.
Split insemination works best when:
- The donor’s expected egg yield is strong enough to provide viable embryos for both partners.
- Both partners want to be genetic parents to children who share the same egg donor.
- The couple is comfortable with the possibility that embryo numbers or quality may differ between them.
- Both partners have healthy sperm.
This method requires clear communication and alignment on how outcomes will be handled. For more on shared cycle planning, see our article on Shared vs. Separate Egg Donor Cycles: A Guide for Gay Dads.
Mixing sperm
In this method, sperm from both partners are combined and used to fertilize the eggs. While this might sound simple in theory, the reality is a bit more technical and not always recommended by fertility doctors.
When sperm is mixed, you won’t know in advance which partner’s sperm fertilized which egg. If conventional IVF is used (where sperm are placed near each egg in a petri dish), the fertilization process is less controlled. With ICSI (intracytoplasmic sperm injection), where a single sperm is injected into an egg, embryologists can alternate which partner’s sperm they use for each egg—but that typically becomes a form of split insemination, not true mixing.
Why some couples consider mixing:
- They want to leave the outcome to chance, without assigning biological parentage in advance.
- They’re drawn to the idea of removing choice as a factor, viewing randomness as a way to share parenthood equally.
A more controlled version of this approach—Intentional Unknowing—offers a clearer path while preserving the spirit of not assigning parentage in advance.
Intentional unknowing
This approach is gaining traction among gay couples who want both partners to contribute sperm—but prefer not to know which embryo came from whom.
Here’s how it works: Both sperm sources are used to fertilize donor eggs (via ICSI or a similar process). Embryos are labeled without linking them to a specific partner. When it’s time for transfer, the selected embryo is transferred to the surrogate without revealing whose sperm was used. You can ask the doctor to choose an embryo of a specific sex, the highest rated embryo, or to simply choose at random.
Why couples choose this:
- They want to share the parenting experience fully, without one dad being labeled the “bio” parent.
- They want just one child and can’t decide which sperm to use.
- They don’t want the child to be raised with different expectations or assumptions based on biology.
- They’re more interested in building a family together than assigning origin stories.
Couples who choose this path often spend time thinking about whether they’ll tell their child later on, and if so, how. Some do DNA testing down the line, others leave it open-ended, and some decide not to pursue the information at all.
Other considerations
Here are a few other approaches and questions that may come up as you think through sperm selection:
- Alternating children: Some couples decide one dad will contribute sperm for the first child, and the other for the second. This can be done with the same egg donor (if embryos are banked), or with a new donor later.
- Decision based on testing: One partner may carry a genetic condition, or have borderline sperm quality, which influences the choice.
- Emotional preference: Sometimes one partner simply feels more strongly about contributing sperm, while the other feels more connected to the pregnancy, birth, or parenting in different ways.
Questions to ask yourselves
Choosing whose sperm to use can be a surprisingly layered conversation. Here are a few questions that might help surface what matters most:
- Do we both want to contribute sperm now, or does one of us feel more ready?
- Would knowing who’s the biological parent affect how we feel about parenting?
- How important is it to us that siblings share the same genetic background?
- Would leaving the outcome to chance (or not knowing) feel empowering—or uncomfortable?
- If one of us isn’t the biological parent, how do we want to talk about that with our child later?
- If we choose not to know whose sperm was used, how do we plan to navigate questions our future child(ren) may have about their own genetic identity?
Final thoughts
There’s no rulebook for how gay dads should make this decision—and that’s a good thing. Every couple has different values, dynamics, and comfort levels. What matters most is that the process feels respectful and intentional for both of you.
Whether you choose to split the eggs, alternate children, or simply decide together whose sperm to use, this is the beginning of building your family—not a competition, and not a test of fairness. With clear communication and the right support from your clinic and legal team, you’ll land on a plan that reflects what matters most: raising a child you both love, equally and fully.
Find an amazing egg donor at Cofertility
At Cofertility, our program is unique. After meeting with hundreds of intended parents, egg donors, and donor-conceived people, we decided on an egg donation model that we think best serves everyone involved: egg sharing.
Here’s how it works: our unique model empowers women to take control of their own reproductive health while giving you the gift of a lifetime. Our donors aren’t doing it for cash – they keep half the eggs retrieved for their own future use, and donate half to your family.
We aim to be the best egg-sharing program, providing an experience that honors, respects, and uplifts everyone involved. Here’s what sets us apart:
- Human-centered: We didn’t like the status quo in egg donation. So we’re doing things differently, starting with our human-centered matching platform.
- Donor empowerment: Our model empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
- Diversity: We’re proud of the fact that the donors on our platform are as diverse as the intended parents seeking to match with them. We work with intended parents to understand their own cultural values — including regional nuances — in hopes of finding them the perfect match.
- Embryo Guarantee: We’re committed to helping your family grow, and proud to offer a generous Embryo Guarantee to every intended parent we work with.
- Lifetime support: Historically, other egg donation options have treated egg donor matching as a one-and-done experience. Beyond matching, beyond a pregnancy, beyond a birth… we believe in supporting the donor-conceived family for life. Our resources and education provide intended parents with the guidance they need to raise happy, healthy kids and celebrate their origin stories.
We are obsessed with improving the family-building journey — today or in the future — and are in an endless pursuit to make these experiences more positive. Create a free account to get started today!

Shared vs. Separate Egg Donor Cycles: A Guide for Gay Dads
For gay dads pursuing egg donation, one of the first big decisions is whether to share one donor cycle or pursue two. This guide breaks down both paths so you can move forward with clarity and confidence.
Becoming a parent through egg donation and surrogacy is filled with decisions—some exciting, others logistically and emotionally challenging. For gay couples who both want a biological connection to their child or children, one of the first big questions is whether to fertilize eggs from the same cycle (a shared cycle) or do two cycles. There’s no single “correct” approach, and the decision is rarely made in isolation. Cost, medical considerations, emotional preferences, and long-term family planning all play a role.
This article unpacks the pros and potential drawbacks of both shared and separate egg donor cycles. We'll cover how a shared cycle works and what makes it appealing, what to expect with separate cycles, and the key factors—personal, financial, and medical—to consider before making a choice. If you're a gay dad or couple weighing your options, this guide is designed to help you make a confident, informed decision.
What is a shared cycle?
In a shared cycle, you and your partner work with one egg donor who completes (or has completed) a single retrieval. The eggs from that retrieval are then divided between both dads. Each partner’s sperm fertilizes their half of the eggs, resulting in two sets of embryos—one per dad—created from the same donor.
This option is common among gay couples who want both partners to have a biological connection to the family. It’s often seen as the most efficient way to include both dads, especially when working with a high-quality donor.
Why couples choose this path:
- It’s usually more affordable. Since you’re only paying for one donor cycle, you share costs like donor compensation, medications, legal work, and the retrieval procedure.
- Embryos will share the same egg donor DNA. For families who value a genetic link between siblings, this can be meaningful.
- The process can feel more unified. Some couples prefer the simplicity of planning one shared timeline.
Potential drawbacks:
- Egg quantity is limited. Even with a strong donor, a single cycle may not yield enough mature eggs to split and still result in a healthy number of embryos for each dad.
- Outcomes can differ. One dad may end up with more or higher-quality embryos than the other, depending on how each sperm source performs.
- Less flexibility for future siblings. If you hope to have multiple children and use embryos from both partners, you may need to be strategic, or end up doing additional cycles later.
What is the two-cycle approach?
In this scenario, the same egg donor completes two separate retrievals. One retrieval’s eggs are fertilized with one dad’s sperm, and the second retrieval’s eggs with the other dad’s. Some couples choose to split both cycles evenly, especially if the number of eggs retrieved varies between cycles, to help ensure fairness and balance.
This option gives each partner a full allocation of eggs to work with, which typically results in more embryos overall and more options for future transfers.
Why couples choose this path:
- Higher embryo yield. Each dad has access to an entire cycle’s worth of eggs, which boosts the chances of having multiple high-quality embryos.
- More flexibility. If one partner’s embryos lead to a pregnancy and the other’s don’t, you still have embryos from both. You can also plan for future siblings with fewer limitations.
- Better balance. With two cycles, you’re less likely to end up in a situation where one partner gets significantly more embryos than the other.
Potential drawbacks:
- It costs more. You’re doubling up on egg donor expenses, including medications and clinic fees. It’s a significant investment.
- It takes more time. If you decide to go with a fresh egg donor cycle, not every donor can or wants to do two back-to-back cycles.
How to think about cost
A shared cycle is typically the lower-cost route. You’re covering one retrieval, one set of medications, and one legal process, and you’re splitting those costs between partners. That can make it a strong option for couples with budget limitations or those early in the family-building process. While it may cost slightly more to create embryos with two sperm sources, it is still the lower cost option if enough embryos are created from a single shared cycle than if a second cycle is needed.
That said, the two-cycle approach might make more sense financially if your long-term goal is multiple children and you want to reduce the chance of needing another donor cycle down the line. While more expensive upfront, it can offer more embryos, fewer unknowns, and potentially fewer emotional or financial surprises later.
Embryo numbers and long-term planning
One key question is how many children you’re hoping to have—and whether you want each dad to have a biological connection to at least one child.
If you’re hoping for:
- One child total, a shared cycle might be enough.
- One child from each partner, it depends on how many embryos result from each half of the split.
- More than two children, or the option to try multiple transfers from each partner’s embryos, a two-cycle approach usually provides more security.
Your clinic can walk you through typical fertilization and blastocyst rates for egg donors and help you model what to expect from a single vs. dual cycle plan. Once you’ve matched with an egg donor, their specific biomarkers (such as her AMH, AFC, and age) can give your doctor additional insight into how many eggs a single cycle may yield, which can help inform your decision-making process around which path is right for you.
Fairness and emotional balance
One reason many couples pursue two separate cycles is to ensure both partners feel equally included, biologically and emotionally. A two-cycle structure gives each dad a full set of eggs, which can make the process feel more balanced from the start. Even if one partner ends up with more or higher-quality embryos, the intent was equitable. That matters for many families.
Shared cycles, on the other hand, can bring more variability. If one partner ends up with significantly fewer embryos—or none—it can lead to difficult conversations or unexpected grief. That doesn’t mean shared cycles are a bad choice, but it does mean couples should talk openly ahead of time about how they’ll handle uneven outcomes.
Some couples navigating a shared cycle choose what’s often referred to as “Intentional Unknowing”. In this approach, sperm from both partners is used to fertilize the donor eggs, and embryos are created without labeling which embryo came from which dad. When it’s time to transfer, embryos are selected and transferred to the surrogate without knowing whose sperm was used to create them. Parentage is discovered only if genetic testing is done later—or not at all.
This method isn’t for everyone, but it appeals to some couples who want just one child, or who want to fully share in the parenting experience without assigning more weight to one biological link over another. It can reduce pressure and reframe the process as one of shared intent rather than genetic outcome. If you’re considering this, talk to your clinic early. Not all programs support it, and it requires careful planning, especially if embryo testing (PGT) is involved.
No matter which path you take, fairness is about emotional clarity, shared expectations, and mutual respect. The more you talk through those pieces before retrieval, the smoother things tend to go later.
Bottom line
There’s no single blueprint for how gay dads should structure egg donor cycles. A shared cycle might be the perfect fit for some families, especially when budgets are tighter or priorities are aligned. For others, two separate cycles offer a stronger sense of balance and long-term flexibility, even if they come with more cost and time.
Whatever you choose, the most important thing is that the decision reflects your values, your partnership, and your goals as future parents. There are many ways to build a family, and what matters most is that it feels right to you.
Read more:
- Gay Men Having Babies: Four Genetic Options with Donor Eggs
- Preparing for Parenthood as a Gay Couple Using Donor Eggs: Tips from a Fertility Psychologist
- Surrogacy Questions Gay Dads Should be Asking
- 8 LGBTQ+ Friendly Fertility Doctors
- How Hopeful Gay Dads Decide Whose Sperm to Use

What To Expect At Your Match Meeting: A Guide For Intended Parents
In this guide, we’ll walk intended parents through what typically happens during a Match Meeting with an egg donor, how to prepare, and how to approach the conversation in a way that helps everyone feel comfortable.
Meeting the person who may help you build your family can bring up all kinds of emotions—excitement, nervousness, hope, and maybe even a little uncertainty about what to say or how it will go. In Cofertility’s Split program, your Match Meeting is a chance to connect with the egg donor who may be donating half of her eggs while freezing the other half for her own future use. It’s not a formal interview; it’s a conversation between two people who’ve been thoughtfully matched and are now getting to know each other.
In this guide, we’ll walk through what typically happens during a Match Meeting, how to prepare, and how to approach the conversation in a way that helps everyone feel comfortable. While every meeting is unique, most follow a familiar rhythm—starting with introductions, then moving into shared interests, questions, and perspectives on the process ahead. Our goal is to help you feel grounded and supported every step of the way.
What’s a Match Meeting?
A Match Meeting is a casual video or phone call between you and the Split member you’ve matched with. These meetings can last from 30-60 minutes and are facilitated by your Cofertility Member Advocate, who will guide the discussion and make sure everyone feels at ease.
The meeting is designed to give both parties a chance to connect beyond written profiles. You’ll get to hear a bit about what brought her to Cofertility and egg sharing, and you’ll have the opportunity to share your own background and what led you here as well. Some people talk about their hobbies, career paths, or family life. Others open up about their hopes for the process, what they’re nervous about, or how they feel about potential future contact.
While these meetings are optional, most intended parents and donors choose to participate, and many tell us that it helped deepen their connection and gave meaning to the match.
Preparing for the meeting
You’ve already reviewed the donor’s profile and spoken with your Member Advocate about why the match may be a good fit. The Match Meeting is an opportunity to bring that profile to life. Think about what aspects of her story stood out to you, and consider what you’d like her to know about you and your family in return.
It’s okay if you’re feeling a little anxious. Many donors feel the same way—everyone wants to make a good impression, and everyone hopes the conversation will feel natural. The good news is: it usually does.
A few ways to prepare:
- Choose a quiet, private space for the call
- Test your Zoom or phone setup in advance
- Make sure you are comfortable with the display name as it will be visible to all participants.
- Consider 2–3 questions you’d like to ask her
- Think about what you feel comfortable sharing about your own story
Your Member Advocate will be there the whole time to guide the flow of conversation and can help navigate any moments of uncertainty or silence.
What to expect during the meeting
The call will begin with brief introductions. Your Member Advocate will often start with a few light prompts to ease into the conversation—like where you’re all calling from, your favorite weekend activity, or what drew you to Cofertility.
Once the conversation starts, it usually flows naturally. Some people click right away over shared interests or life stages. Others take a little longer to warm up, which is also completely normal.
Here’s what’s typical:
- The meeting lasts between 30–60 minutes
- The tone is conversational, not clinical
- Both parties are encouraged to share and ask questions
- The Member Advocate ensures balance and comfort
If you find yourselves really connecting and need more time, your Member Advocate may offer to schedule a second meeting so the conversation doesn’t feel rushed. It isn’t uncommon for intended parents and donors to schedule another meeting a bit further into the match to reconnect, especially after major milestones like medical clearance or finalizing the legal agreement, as the shared goal of the retrieval cycle approaches.
Common topics of discussion
Each Match Meeting is unique, but there are themes that come up often. Some meetings are more emotional, especially if fertility struggles are still fresh. Others feel light, optimistic, or even funny. All of these are valid.
Topics often include:
- What brought each of you to Cofertility
- What excites the donor about egg sharing
- Hobbies, education, or work
- Hopes or goals for the match
- Perspectives on future contact or updates
You don’t need to prepare a script—but it can help to think ahead about how you’d answer a question like, “What does this process mean to you?”
Making the most of your meeting
Good conversations usually happen when both people feel seen and respected. You don’t have to share every detail of your fertility history unless you want to, and you don’t need to try to “win someone over.” Just be yourself.
It’s okay to feel vulnerable. Many donors report feeling more connected to the experience when they hear a bit about the people they’re helping. If it feels comfortable to share, it can add meaning to the match.
You might ask:
- What made you interested in freezing your eggs?
- What stood out to you about the Split program?
- Is there anything you’re excited or nervous about?
And remember: pauses in conversation are totally fine. That’s what your Member Advocate is there for—to keep things moving and make sure everyone feels supported.
What happens after the meeting
Once the meeting ends, you’ll have some time to reflect. You don’t need to decide anything on the spot. Your Member Advocate will check in with you and the donor separately the next day to hear how each of you felt about the call.
If both parties feel good about moving forward, you’ll begin the next steps—clinic coordination, medical screening, and legal documentation. If either side doesn’t feel it’s the right fit, your Member Advocate will guide you through what comes next.
Next steps:
- Reflect on how the conversation felt
- Ask follow-up questions if anything’s unclear
- Let your Member Advocate know how you’d like to proceed
Frequently asked questions
Do we need to talk about our fertility history in detail?
No. You’re welcome to share what feels meaningful to you, but you’re not expected to go deep into your medical background unless you want to. Many donors are open and curious, but respectful of your privacy.
What if I feel emotional during the meeting?
That’s okay. It’s normal to feel a range of emotions—hope, sadness, relief, even gratitude. You’re meeting someone who may help change your life. We’ve seen tears, smiles, and everything in between. Your Member Advocate will support you through all of it.
What should I wear?
For video calls, something that makes you feel comfortable and confident. It’s not a formal meeting—casual or business casual works well. Just aim for something you’d wear to a relaxed coffee with a new acquaintance.
Can I ask about her background or family?
Yes, but keep it conversational. Many people talk about where they grew up, their values, or plans for the future. If there’s something specific you’re curious about and not sure how to ask, your Member Advocate can help guide you. It can be helpful to reach out to your Member Advocate ahead of the call so they can help you gently frame the question, or even find a way to work it into the conversation naturally.
What if we don’t feel aligned?
If something feels off or you’re unsure, that’s okay. Match Meetings are designed to confirm alignment, not to pressure anyone into moving forward. If you decide not to continue with the match, we’ll support you in finding the right fit. We want each match to be as fulfilling as possible for all parties.
Summing it up
Your Match Meeting is a meaningful step in the egg sharing process, but it’s also just a conversation. No one expects perfection—just honesty, curiosity, and openness. Many intended parents tell us this meeting helped them feel more grounded and hopeful about what’s ahead.
Whether the conversation is light or emotional, whether you’re talkative or more reserved, what matters most is that you show up as yourself. Your Member Advocate is there to guide you, and Cofertility is here to support you through every step that follows.
.png)
Why Egg Donor Age Matters (And Why It Doesn't)
While there isn’t a perfect age, there is an ideal age range to optimize for a successful cycle. In this article, I'll share what you need to know about how the age of the egg donor impacts your chances of success. We'll look at the biological factors that influence egg quality, explore recent research that challenges common assumptions, and discuss other important considerations beyond age. By understanding these factors, you'll be better equipped to make an informed decision when selecting an egg donor for your family.
I'm often asked by intended parents about the ideal age for egg donors. They want to know how much the age of the egg donor matters when it comes to donor egg IVF. Should they focus on finding a donor in her 20s? Is early 30s okay? While there isn’t a perfect age, there is an ideal age range to optimize for a successful cycle.
In this article, I'll share what you need to know about how the age of the egg donor impacts your chances of success. We'll look at the biological factors that influence egg quality, explore recent research that challenges common assumptions, and discuss other important considerations beyond age. By understanding these factors, you'll be better equipped to make an informed decision when selecting an egg donor for your family.
The sweet spot for egg donor age
The best age range for donor eggs typically falls between 21 and 34 years old. Here's why:
Peak fertility
From a purely biological standpoint, women in their early 20s through early 30s are generally at the height of their reproductive health. During this time:
- Egg quality is typically at its best
- The risk of chromosomal abnormalities is lower
- Ovarian reserve is usually more robust
Emotional readiness
Donors in their mid-20s to early-30s are also more likely to be emotionally prepared to become an egg donor than younger women. This is a huge decision, and it’s important that egg donors understand the impact of their donation and can confidently follow through on the procedure. Here’s what we mean by emotional readiness:
- Making informed decisions about donation
- Understanding the long-term implications of the process
- Reliably following medical protocols
Donor age vs AMH
As long as an egg donor is between the ages of 21-34, her AMH level will be more predictive of success than her age. AMH is an excellent predictor of ovarian response, and your fertility doctor will use the egg donor’s AMH levels (amongst other biomarkers) to determine the drugs and dosages during the procedure.
Younger donor eggs may not always be better
While the conventional wisdom often leans towards younger donors, recent research has provided some interesting insights that challenge this assumption:
A study focusing on infertility patients using donor eggs found that the chances of live birth were actually 13% lower for cycles using donors under 25 years old compared to those using donors aged 25 to 29.
An older but extensive study involving 3,889 fresh donor egg cycles revealed that donors aged 30 to 34 had a higher incidence of live birth than both younger donors (under 30) and older donors (over 34).
These findings suggest that the relationship between donor age and successful outcomes is more complex than simply "younger is better."
The good news is that the number of eggs retrieved - for donors at any age - is predictable. When you find a donor profile that resonates with you, your fertility doctor can help determine if she’s a good candidate.
Age limits in practice
American Society for Reproductive Medicine (ASRM) suggests that egg donors be at least 21 years of age at the time of donation. Most clinics and agencies like Cofertility follow this suggestion to ensure the donor is mature enough to understand the procedure and follow through on the commitment.
While there is no legal maximum age to become an egg donor, ASRM recommends that donors be under the age of 34 and most clinics follow this guideline. At Cofertility, we require our Split program members to be 33 or under.
Factors beyond age
While age is a significant factor, it's not the only consideration when selecting an egg donor. Other important aspects include:
1. Overall health: A donor's general well-being can impact egg quality
2. Family medical history: This can provide insights into potential genetic factors
3. Lifestyle choices: Habits like smoking or excessive alcohol consumption can affect egg quality
4. Fertility indicators: Measures like AMH levels and antral follicle count offer more precise fertility information
5. Fit for your family: Most importantly, you’ll want to find a fit that feels right for your family.
All the donors at Cofertility are pre-qualified. Read more in How does Cofertility Screen Egg Donors?
The bottom line
While the biologically optimal age for donor eggs is generally between 21 and 34, the "best" age can vary depending on individual circumstances and priorities. At Cofertility, we carefully screen all potential donors, ensuring that regardless of age, they meet high standards for health and fertility.
Remember, the goal is to find the right donor for your family. Our team is here to support you through this process, providing the information and support you need to make an informed decision.
Choosing an egg donor is a big step in your family-building journey. By understanding the role that age plays in egg quality and donor suitability, you're better equipped to navigate this complex but rewarding process. We wish you the best of luck!
Read more:

Cofertility’s Fresh Vs. Frozen Egg Donation Program: Which is Right for Me?
If you’re embarking on the donor egg IVF journey as an intended parent, one of the first decisions you'll face is whether to do a fresh or frozen egg donation cycle. At Cofertility, we offer both options, each with its own unique advantages.
If you’re embarking on the donor egg IVF journey as an intended parent, one of the first decisions you'll face is whether to do a fresh or frozen egg donation cycle. At Cofertility, we offer both options, each with its own unique advantages. But before we dive into the specifics of our fresh and frozen egg donation programs, it's important to highlight a few key aspects of the Cofertility model and experience that remain constant, regardless of which path you choose.
First and foremost, every donor at Cofertility participates in our unique egg sharing model. Instead of receiving cash compensation, Cofertility donors complete a split cycle in which they keep half of the mature eggs retrieved, and donate the other half to intended parents. This means that our donors aren't motivated by financial compensation, but rather by the opportunity to help your family today alongside their own future family building goals. It's a win-win situation that ensures our donors are genuinely committed to the process and aligns their interests with those of intended parents.
Secondly, no matter which program you opt for, you'll be protected by our Embryo Guarantee. While the scope of the guarantee varies with our fresh versus frozen donation programs, know that everyone on our team is deeply committed to helping you achieve your dream of parenthood, and this guarantee reflects that commitment.
Third, regardless of the program you choose, you’ll have the option to decide between having a disclosed or undisclosed relationship with the egg donor. You can also meet with the donor in either program, though the timing of that meeting varies based on whether you go fresh or frozen.
With these promises in place, let's explore the specific features of our fresh and frozen programs to help you determine which path might be the best fit for your family-building journey.
Cofertility’s frozen egg donation program
Matching with a donor in our frozen egg donation program offers several benefits that make it an attractive option for many intended parents.
Increased certainty
A significant advantage of matching with a donor in our frozen program is the increased certainty it brings to the egg donation process. When you match with a donor in our frozen program, she will have already completed her initial retrieval. With things like genetic testing results and psych clearance in hand, this means fewer unknowns and a smoother path forward.
But what does this mean for you in practical terms? It means less waiting, less anxiety, and more confidence in the process. You'll know from the start that your chosen donor has met all medical requirements to donate, reducing the risk of last-minute surprises or disappointments. This can be particularly reassuring for intended parents who have experienced setbacks in their fertility journey and are seeking a more predictable path forward.
Speed
If time is of the essence in your family-building journey, matching with donors participating in our frozen program might be a great fit. Since the time-consuming screening process is complete, the period from matching to embryo creation can be significantly shorter. This is particularly beneficial if you're eager to transfer embryos as soon as possible.
With a fresh egg donation cycle, you might wait one to three months for your donor to complete all necessary screenings and synchronize her cycle with yours. When you match with a donor in our frozen program, you could potentially be ready to create embryos within days of matching. For many intended parents, especially those who feel that time is of the essence, this acceleration of the process can be a game-changer.
Fixed cost transparency
Matching with a donor in our frozen program comes with a clearly defined fixed cost. This includes all expenses related to the donor’s retrieval and screening. Because the cycle has already been completed, you’ll know exactly what you're committing to. This predictability simplifies financial planning and lets you move forward fully informed about the costs involved.
Cofertility’s fresh egg donation program
Matching with a donor from our fresh egg donation program also has its own unique benefits that many intended parents find appealing.
Fresh egg embryo creation
One of the primary advantages of fresh egg donation is the ability to create embryos immediately upon egg retrieval. Some doctors prefer to fertilize fresh eggs vs. previously frozen eggs. This is because it could potentially lead to a higher number of healthy embryos, as it eliminates the need for egg thawing, a process that can sometimes result in the loss of some eggs.
Every egg is precious in this process. So while freezing techniques have advanced significantly in recent years, with vitrification there's still a small chance that some eggs may not survive the thawing process. With fresh eggs, you're working with eggs in their most viable state, potentially increasing your chances of creating healthy embryos.
Local cycles and continuity of care
When you match with a donor from our fresh egg donation program, you have the option of having that donor cycle at your clinic under the care of your own doctor. If you've already established a strong relationship with your fertility team, this ensures continuity throughout the entire process, from egg retrieval to embryo transfer.
This continuity can be incredibly valuable. Your fertility team already knows your medical history, understands your specific situation, and has likely built a rapport with you. Being able to continue working with them through the egg donation process can provide an added layer of comfort and familiarity during what can be an emotionally charged time.
Additionally, having the egg retrieval performed at your local clinic means you have more control over the process. You can be present (if you choose) on the day of the retrieval, adding to the sense of involvement and connection to the process.
A chance to meet the donor before the match is official
With either program, you’ll have the option of having a disclosed or undisclosed donation and can choose to meet the donor if that’s something both parties are interested in.
However, if you’re interested in matching with a donor from our fresh program, you’ll have the unique opportunity to potentially meet with the donor before she begins her cycle as part of our mutual matching process. This can be a meaningful experience for intended parents who value this personal connection from the outset.
For some intended parents, meeting the donor before the retrieval can help solidify their choice and create a sense of connection to the process. It can be an opportunity to express gratitude, ask questions, or simply put a face to the generous individual who is helping to make your dreams of parenthood a reality.
It's important to note, however, that this meeting is entirely optional. We understand that every intended parent and egg donor has different comfort levels when it comes to donor contact, and we respect whatever level of interaction you prefer.
Making your decision: it's all about finding your perfect match
Ultimately, for many intended parents, the choice between our fresh and frozen programs often comes down to finding the right donor. Both programs have their merits, and the best choice for you will depend on your specific circumstances, preferences, and the connection you feel with potential donors.
If you're open to either journey, we recommend exploring both options. You might find that you connect deeply with a donor in our fresh egg donation program, or you might discover that the perfect donor for you has already completed her cycle as a part of our frozen egg donation program.
Consider your priorities:
- Is time a critical factor for you? If so, frozen egg donation might be your best bet.
- Do you feel strongly about using fresh eggs? Then fresh egg donation could be the way to go.
- Is the ability to meet your donor before the retrieval important to you? With donors in our fresh egg donation program, you could have this opportunity.
- Regardless of which path you choose, all Cofertility intended parents are covered by our Embryo Guarantee.
At Cofertility, we're committed to supporting you through every step of your journey, regardless of which program you choose. Our team is here to answer your questions, address your concerns, and help you navigate this important decision.
Remember, this is your journey. Trust your instincts, ask questions, and don't hesitate to reach out to our team for guidance. We're here to help you navigate these decisions and find the path that feels right for you.
In the end, whether you go fresh or frozen, what matters most is the family you're building and the love that will fill your home. That is the most beautiful outcome of all. Your future child won't care whether they came from fresh or frozen eggs – they'll just be thrilled to be part of your family.
So take a deep breath, trust in the process, and know that with Cofertility by your side, you're one step closer to holding your baby in your arms. We’ve got hundreds of incredible donors on our egg donation platform who would love to help you make your dreams of parenthood a reality.

An Intended Parents Guide to Frozen Egg Donation with Cofertility
Everything you need to know about matching with a donor in Cofertility's frozen egg donation program, including the process, benefits, our Embryo Guarantee, and more.
At Cofertility, we believe that everyone deserves the ability to build the family of their dreams. Part of this is ensuring intended parents have access to different options for working with an egg donor, including both fresh and frozen egg donation programs. In this guide, we’ll walk you through everything you need to know about working with a donor in our frozen egg donation program.
If you’re interested in learning more about our options for fresh egg donation, click here.
An overview of frozen egg donation
Our unique egg sharing model provides intended parents with an alternative to cash compensation for egg donation. At Cofertility, we operate based on an egg sharing model where our donors donate half of the eggs retrieved and keep the other half for their own future family planning.
The key difference between fresh and frozen egg donation with Cofertility is the point at which the donor completes her screening and egg retrieval. When you match with a donor in our Frozen program the donor’s screening and retrieval process is completed in advance of matching.
Donors in the frozen egg donation program will undergo the same rigorous screening process as those in our fresh egg donation program. All donors have been pre-qualified to move forward with egg donation per ASRM, FDA, and standard egg donation guidelines. A preliminary screening for donors includes:
- Confirming the donor's age is within ASRM guidelines. All donors on our matching platform are 21-33 years old.
- Reviewing the donor’s personal medical history, including lifestyle, chronic conditions, mental health, and reproductive health, in line with ASRM, FDA, and standard egg donation guidelines.
- Reviewing the donor’s biological family’s medical history, inclusive of evidence of genetic disorders, cancer history, and other conditions and illnesses, in line with ASRM, FDA, and standard guidelines.
- Collecting and reviewing past egg donation history with outcomes, if applicable.
- AMH testing via blood draw. All Cofertility donors are required to have an AMH level of 2.0 or higher.
At the time a donor in our frozen egg donation program is listed on our platform, they will have also already completed additional screening that includes:
- Antral follicle count (AFC) assessment
- General health examination
- Genetic carrier screening
- Psychological screening
Considerations for frozen egg donation
Both fresh or frozen egg donation can be great options, depending on your individual goals and what you’re looking for at this point in time. There are several reasons intended parents may choose to pursue frozen egg donation with Cofertility.
Quicker process
Matching with a donor in our frozen program can provide a unique opportunity to move forward with your family-building plans faster, as frozen eggs can be fertilized or shipped to your clinic immediately. Time from match to embryo creation is a lot faster with frozen since the screening – which is what takes the most time – is already completed. If you’re looking to transfer embryos ASAP, matching with a frozen donor can help make that happen.
Added certainty
Because a frozen donor has completed all of her medical screening and retrieval in advance of matching, it brings a little more certainty to the process. With screening results in hand, you’ll have more certainty over whether a donor is the right fit for your family building goals from the outset which can help alleviate some of the speed bumps or heartaches that may come with a fresh donation journey. Every frozen match is also guaranteed to have a minimum of at least 6 frozen eggs and you'll have visibility into that upfront.
Generous guarantee
The pricing model of the frozen program allows us to put our Embryo Guarantee on the entire cost of the match. If the frozen eggs that you receive do not lead to our guaranteed embryo minimum, we’ll replace those with an equivalent number of eggs for $0. You don’t have to pay for any screening or retrieval fees again. What’s more, our guarantee covers up to three total matches, while other egg banks may provide a single replacement cohort.
Finding the right donor
Ultimately, the most important thing is that you feel great about the donor who you match with. If you’re open to either journey, it might just be a question of finding the right donor and then accommodating whichever program she’s in.
Our Embryo Guarantee
We’re truly committed to helping families grow — that’s why we’ve built one of the most parent-friendly programs out there, inclusive of our Embryo Guarantee.
As noted, if anything outside of your control prevents you from reaching the guaranteed minimum number of blastocyst-stage embryos for your match, we will rematch you at no additional charge until that minimum is met, up to three total matches.
In our Frozen egg donation program, the number of embryos guaranteed is based on the number of eggs in your original match.
How it works
We understand how daunting the process of looking for an egg donor can be. Our team works tirelessly to ensure that the process of finding your perfect match is as straightforward and as positive of an experience as possible. If you are interested in matching with a donor participating in our frozen egg donation program, here’s how the process works:
- Create a free account: Simply answer a few questions about what you’re looking for to get immediate access to our donor matching platform. From there, you’ll be able to view profiles for the hundreds of donors that are available to match with families like yours.
Donors participating in our frozen program will have a note in the “About this donor” section of their profile.
- Find your match: When you find a donor with whom you’d like to match. Just press the “hold this match” button at the top of her profile. From there, you’ll be directed to pay your $500 Match Initiation Fee, which will immediately remove the donor from the platform so no other intended parents can match with her while we confirm details with all parties.
At any time, you can also schedule a free consultation with a member of our team so that we can help you find your match.
- Match kickoff: Shortly after you place a hold on a match, you’ll be assigned a dedicated Member Advocate you will be with you through the process end-to-end. Your Member Advocate will reach out to set up a kickoff call, during which you’ll go over the details of the process and confirm your match preferences.
- Embryo creation: When you match with a donor in our frozen egg donation program, the donor’s screening and retrieval is complete. The next step will be finalizing the number of eggs that you’re receiving and your plans for fertilization.
In our frozen program, donors complete two cycles. All of the eggs from the first cycle are donated while she keeps all of the eggs from the second cycle. The donated portion of the eggs will be stored at our clinic partner where the retrieval is done and can be shipped to your clinic or thawed and fertilized on site.
Depending on the cycle outcome, you will have the option of keeping all of the eggs from that cycle, or keeping a cohort of half of the eggs from that cycle. Our team can let you know upfront how many eggs are available from a given donor and what your options are.
From there, you can ship frozen eggs to your clinic, where they’ll be thawed and fertilized. You can also work with the clinic where the retrieval took place, thawing the eggs and creating embryos onsite. Some intended parents choose to complete PGT on their embryos prior to implantation, while others may not. Some intended parents plan to carry the pregnancy themselves, while others are working with a gestational carrier. In any case, we’re passionate about creating an egg donation experience that is anything but transactional, and we are here to help make the process as seamless as possible — from embryo creation, to pregnancy, birth, and beyond.
Pricing
With the frozen program, you’ll pay a single lump sum fee that varies based on the number of frozen eggs available with the match. The full cost breakdown can be found on our pricing page.
Conclusion
At Cofertility, we know there’s no one-size-fits-all approach to growing your family with donor eggs. We’re proud to offer our unique no-cash compensation egg sharing model for both fresh and frozen donation to give intended parents as many paths as possible to grow their families. To create a free account and get instant access to our donor matching platform, click here. We can’t wait to be part of your journey.

An Intended Parents Guide to Fresh Egg Donation with Cofertility
Everything you need to know about matching with a donor in Cofertility's fresh egg donation program, including the donation, screening, and retrieval process.
At Cofertility, we believe that everyone deserves the ability to build the family of their dreams. Part of this is ensuring intended parents have access to different options for working with an egg donor, including both fresh and frozen egg donation. In this guide, we’ll walk you through everything you need to know about working with a donor in our fresh program.
If you’re interested in learning more about our options for frozen egg donation, click here.
An overview of fresh egg donation
Our unique egg sharing model provides intended parents with an alternative to cash compensation for egg donation. At Cofertility, our donors always keep half of the eggs retrieved for her own future family planning and donate half to your family.
The key difference between fresh and frozen egg donation with Cofertility is the point at which the donor completes her screening and egg retrieval. With fresh egg donation, the screening and retrieval process is started after you match with the donor.
Rest assured, we complete preliminary screening for donors prior to listing them on our platform, so all donors have been pre-qualified to move forward with egg donation per ASRM, FDA, and standard egg donation guidelines. Initial screening includes:
- Confirming the donor's age is within ASRM guidelines. All donors on our matching platform are 21-33 years old.
- Reviewing the donor’s personal medical history, including lifestyle, chronic conditions, mental health, and reproductive health, in line with ASRM, FDA, and standard egg donation guidelines.
- Reviewing the donor’s biological family’s medical history, inclusive of evidence of genetic disorders, cancer history, and other conditions and illnesses, in line with ASRM, FDA, and standard guidelines.
- Collecting and reviewing past egg donation history with outcomes, if applicable.
- AMH testing via blood draw. All Cofertility donors are required to have an AMH level of 2.0 or higher.
Upon confirming a mutual match between you and the donor, additional screening will be initiated to include:
- Genetic carrier screening - initiated immediately upon match
- Antral follicle count (AFC) assessment
- General health examination
- Psychological screening
Once the donor completes the necessary screening and receives your doctor’s approval to move forward as a donor, you’ll enter into a legal agreement directly with the donor. From there, the egg retrieval process will begin.
Considerations for fresh egg donation
Both fresh or frozen egg donation can be great options, depending on your individual goals and what you’re looking for at this point in time. There are several reasons intended parents may choose to pursue fresh egg donation with Cofertility.
Embryo creation from fresh eggs
One of the main perks of fresh egg donation is that embryos can be created immediately upon retrieval, rather than being created from previously-frozen eggs. This could potentially lead to more healthy embryos being successfully created, since the thawing process can lead to a loss of some eggs.
Local cycles
Additionally, working with a donor in our fresh program allows for the opportunity to have the donor cycle at your clinic, potentially even with your doctor. If you have already established a great relationship with your doctor and their team, this can ensure continuity throughout the entire process.
Meeting the donor pre-retrieval
While both programs allow you to meet with the donor (and both allow for disclosed or undisclosed donations), with fresh egg donation, you can meet with the donor in advance of her completing her retrieval cycle.
Finding the right donor
Ultimately, the most important thing is that you feel great about the donor who you match with. If you’re open to either journey, it might just be a question of finding the right donor and then accommodating whichever program she’s in.
Our Embryo Guarantee
We're committed to helping your family grow: that's why we back every Cofertility match with our comprehensive Embryo Guarantee.
In our Fresh program, all intended parents are guaranteed at least two blastocyst-stage embryos.
If anything outside of your control prevents you from reaching this minimum number of blastocyst-stage embryos, we will rematch you at no additional charge until that minimum is met, up to three total matches.
How it works
We understand how daunting the process of looking for an egg donor can be. Our team works tirelessly to ensure that the process of finding your perfect match is as straightforward and as positive of an experience as possible. If you are interested in matching with a donor participating in our fresh egg donation program, here’s how the process works:
- Create a free account: Simply answer a few questions about what you’re looking for to get immediate access to our donor matching platform at no cost. From there, you’ll be able to view profiles for the hundreds of donors that are available to match with families like yours. All donors listed on our platform are available for fresh donation unless noted otherwise in the “About this donor” section of her profile.
- Find your match: When you find a donor with whom you’d like to match. Just press the “hold this match” button at the top of her profile. From there, you’ll be directed to pay your $500 Match Initiation Fee, which will immediately remove the donor from the platform so no other intended parents can match with her while we confirm details with all parties.
At any time, you can also schedule a free consultation with a member of our team so that we can help you find your match.
- Mutual match confirmation: Shortly after you place a hold on a match, you’ll be assigned a dedicated Member Advocate who will be with you through the process end-to-end. Your Member Advocate will reach out to set up a kickoff call, during which you’ll go over the details of the process and confirm your match preferences. At the same time, the donor will go through the same process, to ensure a mutual match all around.
Additionally, if both parties are interested, we can facilitate a virtual or in-person meeting between you and your donor. This can be done on- or off- camera and with or without names revealed, in order to accommodate both disclosed and undisclosed matches.
- Donor screening and retrieval: Once the match is confirmed by you and the donor, we’ll get started on coordinating the donor’s in-person screening. This can be done either at your clinic (you’ll be responsible for paying for the donor’s travel expenses) or at a clinic local to the donor. Once all screening results are in and we receive approval from your doctor, you’ll work with an attorney who will draft a legal agreement between you and the donor. Once there’s legal clearance, the donor’s retrieval cycle will be scheduled.
- The split and embryo creation: On the day of the donor’s retrieval, the mature egg yield will be split evenly between both parties (if there is an odd number of mature eggs retrieved, you will receive the “extra” egg). The donor’s portion of the eggs retrieved will be immediately frozen and put into long term storage. Most intended parents choose to create embryos immediately upon retrieval, but you’ll also have the option to freeze unfertilized eggs, if preferred.
Post-embryo creation, what happens next is entirely up to you. Some intended parents opt to complete a fresh embryo transfer, while others may decide to freeze and store embryos for later use. Some intended parents choose to complete PGT on their embryos prior to implantation, while others may not. Some intended parents plan to carry the pregnancy themselves, while others are working with a gestational carrier. In any case, we’re passionate about creating an egg donation experience that is anything but transactional, and we are here to help make the process as seamless as possible — from embryo creation, to pregnancy, birth, and beyond.
Pricing
With a fresh cycle, you can expect to pay the Match Initiation Fee, Cofertility’s Coordination Fee, and a range of expenses to various third parties involved in the process, including lawyers, genetic counselors, and your clinic. We break this down in more detail on our pricing page.
Conclusion
At Cofertility, we know there’s no one-size-fits-all approach to growing your family with donor eggs. We’re proud to offer our unique no-cash compensation egg sharing model for both fresh and frozen donation to give intended parents as many paths as possible to grow their families. To create a free account and get instant access to our donor matching platform, click here. We can’t wait to be part of your journey.

What the Recent Supreme Court Ruling in Alabama Means For Donor Egg IVF
Understand the far-reaching effects of the recent Alabama Supreme Court ruling on donor egg IVF. Learn about the legal ramifications, implications for fertility care, and discover resources available to those affected.
This article was last updated on March 1, 2024. The Alabama Supreme Court ruling is a quickly unfolding situation. Be sure to consult official news sources or legal experts for the most up-to-date information and guidance.
On February 16th, 2024, the Alabama Supreme Court ruled that frozen embryos can be considered children under state law, a ruling that sent shockwaves through the reproductive health community and raised widespread concerns regarding its potential impact on fertility care. Several of the state’s in vitro fertilization (IVF) clinics have since paused services, and lawmakers, doctors, and patients are raising concerns about the far-ranging impacts of the ruling on healthcare and reproductive technology.
While there’s still a great degree of uncertainty, in this article, we'll delve deeper into the implications of this significant legal shift, exploring how it specifically impacts donor egg IVF procedures. Additionally, we'll explore what resources may be available to those affected by this ruling and provide insights on how you can engage in advocacy efforts to address these challenges.
What is the Alabama court case about?
The recent ruling by the Alabama Supreme Court was the result of a lawsuit filed by three couples who underwent IVF treatment at a fertility clinic in Alabama. Following successful IVF procedures that resulted in the birth of healthy babies, the couples, like many undergoing such treatments, had additional embryos preserved by the clinic which was located inside of a hospital.
However, in December 2020, a patient at the hospital gained unauthorized access to the fertility clinic's cryo-preservation unit and mishandled the frozen embryos, resulting in their destruction. This tragic incident led the plaintiffs to file lawsuits against both the fertility clinic and the hospital where it was located.
One of the lawsuits centered around the application of Alabama's Wrongful Death of a Minor Act. Initially dismissed by the trial court, which ruled that embryos in vitro did not qualify as minors under the act, the case was escalated to the Supreme Court of Alabama. The Alabama Supreme Court diverged from the trial court's stance. They asserted that the Wrongful Death of a Minor Act applied to all unborn children, regardless of their location—in utero or in vitro—at the time of the incident. By deeming the in vitro embryos as persons under the law, the court allowed the couples to proceed with their lawsuit, seeking punitive damages for what they perceived as the wrongful death of their children.
What are the implications for Alabama fertility patients?
The recent ruling by the Alabama Supreme Court does not explicitly impose any bans or restrictions on IVF procedures. However, legal experts suggest – and we’re already seeing in practice – that the decision may create confusion regarding the legality of certain aspects of IVF within Alabama.
For context, data from the Centers for Disease Control and Prevention indicates that approximately 2% of babies in the United States are conceived using assisted reproductive technology. Among the various treatments available, IVF stands out as the most commonly utilized method. IVF is a complex procedure that begins with a stimulated cycle wherein a woman undergoes hormone injections to prompt her ovaries to produce numerous eggs. These eggs are then harvested and united with sperm, giving rise to embryos that undergo incubation for development.
After a few days, the embryos undergo assessment, with only the most viable ones selected for transfer into the woman's uterus. The goal is for the transferred embryo to implant successfully, leading to a healthy pregnancy and ultimately the birth of a child. Any surplus high-quality embryos from the stimulated cycle are typically cryopreserved for potential future use. Not all harvested eggs are suitable for fertilization and not all embryos may be deemed suitable for transfer. Subpar-quality eggs, abnormally fertilized embryos, and embryos displaying poor quality are routinely discarded as part of the process.
The crux of the matter in the recent ruling lies in the classification of embryos as persons under Alabama law. This designation has already raised significant questions regarding the permissible usage and storage of embryos by fertility clinics. In essence, the interpretation of Alabama law equates the legal protection of frozen embryos to that of living children. Under this interpretation, individuals who inadvertently or intentionally destroy a frozen embryo in Alabama could potentially face severe penalties, including manslaughter or murder charges.
This ruling has the potential to significantly disrupt access to fertility care as it may introduce additional regulatory burdens in an already complex medical landscape and could potentially drive up procedural costs. Although the extreme of the financial implications remains unclear, factors such as additional storage fees and liability expenses may further contribute to the rise in expenses.
On top of existing clinics closing, the ruling might lead to a reduction in IVF providers in the state. Even if clinics reopen, fertility doctors may be hesitant to practice in or relocate to Alabama. In light of the perceived risks tied to freezing or destroying embryos within this legal framework, fertility clinics across the state are already proceeding with caution, opting to restrict their IVF services, including retrievals and cryopreservation. Consequently, patients are already finding themselves compelled to seek treatment outside of Alabama, a situation that might intensify if clinics can’t get back to operating at full capacity.
How does this affect donor egg IVF?
Egg donation itself is not in as much legal limbo as eggs are not considered fetuses under current law. However, given the end goal of fertilizing and transferring the donor eggs, the ruling of course affects the donor egg IVF process.
Donor egg IVF encompasses several stages, including egg retrieval, fertilization, and subsequent embryo transfer to the intended parent's or surrogate's uterus. This ruling may necessitate procedural changes in IVF, potentially influencing the number of embryos created and transferred per cycle. Moreover, frozen embryo transfers are commonly utilized in donor egg IVF for preimplantation genetic screening. The ruling could introduce additional regulations or restrictions on the use of frozen embryos.
Many individuals and couples pursuing donor egg IVF have already been through lengthy, challenging, and expensive fertility journeys. This is particularly true for LGBTQIA+ individuals and couples who often depend on donor egg IVF to grow their families. In short, the Alabama Supreme Court only introduces more complexity and potential hardship to a landscape that’s already fraught with challenges. Regardless of where someone is in this family-building journey, this ruling has the potential to alter their trajectory.
What resources are available to those impacted and how can I get involved?
In response to these challenges, several organizations have stepped up to support individuals and families in Alabama.
Cofertility's storage partner, TMRW Life Sciences, is offering one year of free cryostorage for frozen eggs and embryos to patients who live in Alabama and who wish to move their embryos to TMRW’s biorepository in NYC.
Conceive is offering a free one-month membership to Conceive Premium for anyone in Alabama. Conceive Premium provides invaluable assistance and guidance throughout your fertility journey by offering 24/7 support from fertility nurses, peer coaching, community forums, and more.
Furthermore, there are various ways individuals can get involved with advocacy efforts aimed at supporting Alabama families and protecting IVF access across the country. You can show your support for organizations that fight to uphold reproductive rights and ensure equitable access to fertility treatments like the American Society for Reproductive Medicine (ASRM) and RESOLVE, the National Infertility Association. To stay in the loop, sign up for alerts from RESOLVE’s Advocacy Network and follow @resolveorg on Instagram.
Sharing personal stories through public channels like social media can help raise awareness and amplify the voices of those affected. You can also use easily-accessible, online forms to send a letter to Congress and encourage them to address the issue. Lastly, local support groups, such as RESOLVE peer-led support groups in Alabama, provide a supportive environment for individuals to connect with others facing similar challenges.
Cofertility’s position
We at Cofertility are deeply concerned about the recent verdict and have been monitoring the situation closely. Our team is diligently tracking developments and working with our legal and professional advisors in order to navigate any potential implications side by side with our members. We understand the importance of safeguarding the rights and interests of donors and intended parents alike.
We believe the decision to seek medical support in family planning is profoundly personal and should be guided solely by patients and their healthcare providers. We believe that access to safe and effective medical care should be available to all individuals on their journey to parenthood, regardless of their location.
As a proactive measure until the law becomes clearer, we are temporarily suspending the facilitation of retrievals in Alabama where legislative uncertainty or restrictions pose potential risks to our members. We are also actively engaging with any intended parents in Alabama to assess their specific situations and explore potential paths forward. We’re focused on providing these members of our community with comprehensive support and guidance as they navigate these challenging times. If you are a Cofertility member and have any questions, concerns, or would like to get in contact with our team to talk through the specifics of your situation and how we may be able to help, please don’t hesitate to reach out.
.png)
Does Donor Egg IVF Increase Chances of Twins?
Does donor egg IVF increase the chances of conceiving twins? In this guide, I’ll dive into the essentials of donor egg IVF, its odds for success, the chances for twins, and the potential risks associated with multiples.
The world of fertility treatments is a rapidly-evolving landscape, teeming with options, intricacies, and promises of renewed hope for LGBTQ+ families as well as those struggling to conceive. Among these treatments, donor egg in vitro fertilization (IVF) has become an increasingly common path, with a substantial 12% of all IVF cycles in the U.S., over 16,000 a year, involving eggs retrieved from a donor.
But does donor egg IVF increase the chances of conceiving twins? In this guide, I’ll dive into the essentials of donor egg IVF, its odds for success, the chances for twins, and the potential risks associated with multiples.
What is donor egg IVF?
IVF with donor eggs is a medical procedure where eggs are collected from a donor, fertilized in a laboratory with the intended father's or a donor's sperm, and the resulting embryo is then implanted in the uterus of the intended mother or a gestational carrier.
This process may be an option for women with diminished ovarian reserve, repeated IVF failure, infertility due to recurrent miscarriage, or those who carry genetic disorders that they do not want to pass on to their children. It is also an option for LGBTQ+ families and single males.
Donor egg IVF typically involves several steps: the selection of an egg donor, extraction and fertilization of the donor eggs, and transfer of the embryo(s). To learn more about the process, check out this article.
What are the odds of getting pregnant with donor eggs?
Success rates for donor egg IVF are often more promising compared to traditional IVF. At Cofertility, for those who match with a donor in our fresh egg donation program, the average number of mature eggs a family receives and fertilizes is 12. The number of eggs retrieved varies by patient and cycle, but can be predicted by a donor’s age, AMH, and antral follicle count, all of which will be known to you after the donor’s initial screening. Qualified candidates have an ample ovarian reserve for both their own needs and sharing. Egg share donors also often work closely with a fertility doctor to determine, based on their own medical history, the optimal number of eggs needed for their own future family-building goals. Should it make sense for the donor, they may choose to pursue a second egg-sharing cycle to maximize the chances of success for everyone.
Matching with a donor in our frozen program can provide the opportunity to move forward with your family-building plans faster, as frozen eggs can be fertilized or shipped to your clinic immediately or as soon as the cycle is complete. Donors undergoing frozen cycles complete equally rigorous ovarian reserve testing. While the total number of frozen eggs available will vary based on the donor’s retrieval outcomes, every frozen match is guaranteed to have a minimum of at least 6 frozen eggs. To learn more about these programs and the differences between them, click here.
Around 53 percent of all donor egg cycles will result in at least one live birth. This percentage varies depending on the egg donor, recipient body mass index, stage of embryo at transfer, the number of oocytes retrieved, and the quality of the clinic.
At every age, the chances of birth with donor eggs is better, but those who benefit the most from donor eggs are women over 35 and those with low ovarian reserve. In fact, about one-quarter of women over 40 who succeeded with IVF did so through the use of donor eggs.

The chart was made using the SART Patient Predictor for an average woman (5’4”, 150 lbs) with diminished ovarian reserve. As you can see, the chances of live birth after one donor egg cycle is 54% for recipients under 40, and only goes down slightly after this.
The advantage is primarily due to the utilization of eggs from younger donors, typically between the ages of 21 and 34.
It’s important to remember that your age when you get pregnant is not as important as the age of the eggs with which you get pregnant. The success of egg donation depends on many factors, but is not considered to be related to the age of the recipient.
Chances of twins with donor eggs
One question we get a lot is the likelihood of conceiving twins with donor egg IVF.
According to the CDC, in 2021 live births from donor egg IVF had a slightly higher chance of twins compared to IVF with a patient’s own eggs.
- General population: 3.2%
- IVF with patient’s own eggs: 5.2%
- Donor egg IVF: 6.0%
- Donor embryo IVF: 7.4%
But as you can see from the data above, IVF (regardless of whose eggs are used) is associated with higher chances of twins.
How does that work? First, the chances of an embryo splitting and becoming monozygotic twins (aka identical twins) is 2.25 times higher with IVF than with unassisted conception.
But twins after IVF are usually due to a patient having more than one embryo transferred to the uterus, making them dizygotic twins. When IVF was just starting out, there was no genetic testing and fertility doctors would transfer multiple embryos at one time. This led to a multiples rate of over 20% for those who underwent IVF. Nowadays, as technology has advanced, single embryo transfers are the norm, and the incidence of twins has gone down drastically.
Can I transfer two donor egg embryos?
The transfer of two embryos is an option in some fertility clinics, and it often increases the chances of pregnancy. However, it's important to consider the associated risks, benefits, and guidelines.
The American Society for Reproductive Medicine (ASRM) recommends that clinicians and patients carefully discuss the number of embryos to be transferred, considering factors like maternal age, embryo quality, and the patient's individual medical situation. In some cases, transferring two embryos may be a viable option, while in others, a single embryo transfer may be the preferred route to minimize the risk of multiples,
Risk of pregnancy with multiples
While the prospect of twins may be appealing to some, there are increased risks associated with multiple pregnancies. Twin pregnancies are associated with higher rates of preterm birth, low birth weight, and maternal complications such as gestational diabetes and preeclampsia.
- Preterm birth, defined as delivery before 37 weeks of gestation, occurs more frequently in multiple pregnancies. Preterm infants may face an array of health challenges, including respiratory distress syndrome, infections, and long-term developmental issues. These risks underscore the importance of careful monitoring during pregnancy and specialized neonatal care following birth.
- Low birth weight, often linked to preterm birth, is a common occurrence in twin pregnancies. Infants born with low birth weight are at increased risk for health problems both immediately after birth and later in life. Challenges may include difficulties with feeding and temperature regulation, as well as potential long-term developmental delays.
- Other complications from twin pregnancies due to added stress on the mother's body can lead to an increased risk of gestational diabetes and preeclampsia, a condition characterized by high blood pressure and damage to organs such as the liver and kidneys. Other potential complications may include an increased likelihood of cesarean section (C-section), excessive bleeding during childbirth, and higher rates of postpartum depression.
You should understand these risks and engage in thoughtful, well-informed planning and decision-making with your fertility doctor if you are considering the transfer of multiple embryos in donor egg IVF.
The bottom line
Donor egg IVF represents a beacon of hope for many aspiring parents. With its relatively high success rate, more and more families are turning to donor eggs to build their family.
However, the decision to pursue this treatment—and whether to transfer one or two embryos—requires careful consideration of the odds, potential risks, and individual medical circumstances. Consulting with fertility doctors, understanding the available scientific data, and considering personal preferences and ethical considerations will equip you to make informed choices on your journey towards parenthood. We wish you all the best!
Learn about egg sharing
At Cofertility, our program is unique. After meeting with hundreds of intended parents, egg donors, and donor-conceived people, we decided on an egg donation model that we think best serves everyone involved: egg sharing.
Here’s how it works: our unique model empowers women to take control of their own reproductive health while giving you the gift of a lifetime. Our donors aren’t doing it for cash – they keep half the eggs retrieved for their own future use, and donate half to your family.
We aim to be the best egg sharing program, providing an experience that honors, respects, and uplifts everyone involved. Here’s what sets us apart:
- Human-centered: We didn’t like the status quo in egg donation. So we’re doing things differently, starting with our human-centered matching platform.
- Donor empowerment: Our model empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
- Diversity: We’re proud about the fact that the donors on our platform are as diverse as the intended parents seeking to match with them. We work with intended parents to understand their own cultural values — including regional nuances — in hopes of finding them the perfect match.
- Embryo Guarantee: We’re committed to helping your family grow, and proud to offer a generous Embryo Guarantee to every intended parent we work with.
- Lifetime support: Historically, other egg donation options have treated egg donor matching as a one-and-done experience. Beyond matching, beyond a pregnancy, beyond a birth…we believe in supporting the donor-conceived family for life. Our resources and education provide intended parents with the guidance they need to raise happy, healthy kids and celebrate their origin stories.
We are obsessed with improving the family-building journey — today or in the future — and are in an endless pursuit to make these experiences more positive. Create a free account to get started today!
.png)
Egg Sharing: Will I Get Enough Eggs?
In this article, we’ll aim to answer that question by exploring the concept of egg sharing, discussing factors that contribute to egg yield, looking at the average number of embryos created, and share how Cofertility can help you realize your dream of growing your family.
Egg sharing programs have become an increasingly popular option for families pursuing donor egg IVF. But if you only get half of the eggs retrieved, will that be enough for a baby?
In this article, we’ll aim to answer that question by exploring the concept of egg sharing, discussing factors that contribute to egg yield, looking at the average number of embryos created, and share how Cofertility can help you realize your dream of growing your family.
What is egg sharing?
Egg sharing is a model where egg donors get to keep half of the eggs retrieved for her own future use, instead of cash compensation.
Why is cash compensation problematic? A 2021 Harvard study found that 62% of donor-conceived adults felt the exchange of money for donor gametes was wrong, and 41% were troubled by the fact that money was exchanged around their conception. By allowing our donors to freeze their eggs as part of the process, our unique model honors everyone involved.
At Cofertility, we exclusively work under the egg sharing model, which we call Split, because we think it’s better for everyone involved – the intended parents, the egg donor, and ultimately the donor-conceived child. Egg sharing empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
Read more in Six Reasons Why Egg Sharing is a Better Egg Donation Model for Intended Parents
Will I get enough eggs in an egg sharing model?
One common question from individuals considering egg sharing is whether they will receive an adequate number of eggs to achieve a successful outcome. A 2003 UK study of egg sharing amongst IVF patients found that participating in an egg sharing program did not compromise the chance of achieving a pregnancy or live birth for the egg sharer or the recipient.
There are several factors that can influence the number and quality of eggs retrieved, such as:
- Donor's ovarian reserve: Even more important than age in predicting egg retrieval outcomes is ovarian reserve, which refers to the quantity of eggs. A higher ovarian reserve indicates a larger pool of eggs available for retrieval and sharing. One way to determine ovarian reserve is an antral follicle count that is done by a doctor. Another biomarker for ovarian reserve is anti-müllerian hormone (AMH). At Cofertility, we only work with egg donors with an AMH over 2.0 ng/mL, to increase the chances of sufficient egg yield.
- Donor’s overall health: The overall health of the egg donor can play a significant role in the number of eggs available for sharing. Donors who maintain a healthy lifestyle, including being a non-smoker, have better reproductive health. Our donors go through rigorous screening to ensure and get medical approval to ensure they are a good egg donation candidate.
- Response to stimulation protocols: Fertility clinics use stimulation protocols involving hormonal medications to stimulate the ovaries and promote the development of multiple mature eggs. The response of the donor's ovaries to these medications can vary, affecting the number of eggs that can be retrieved for sharing.
- Hormone stimulation: Fertility medications, such as follicle-stimulating hormone (FSH), are administered to the donor to stimulate the growth and maturation of multiple eggs within the ovaries. The dosage and duration of hormone stimulation are tailored to each individual to optimize the number of eggs produced. The exact drugs and dosages chosen will impact the outcome, as well as the donor’s adherence to the prescribed medications.
- Ovarian monitoring: Regular monitoring through ultrasounds and blood tests is essential during the stimulation phase. These monitoring sessions help fertility specialists track the growth and development of follicles (fluid-filled sacs containing eggs) and adjust medication dosages if needed. Close monitoring ensures the timely retrieval of mature eggs.
As you can see, many of these items are related to the egg retrieval cycle itself, where outcomes can be influenced by the quality and expertise of the clinic and fertility doctor. Learn more about finding a good IVF clinic.
At Cofertility, for those who match with a donor in our fresh egg donation program, the average number of mature eggs a family receives and fertilizes is 12. The number of eggs retrieved varies by patient and cycle, but can be predicted by a donor’s age, AMH, and antral follicle count, all of which will be known to you after the donor’s initial screening. Qualified candidates have an ample ovarian reserve for both their own needs and sharing. Egg share donors also often work closely with a fertility doctor to determine, based on their own medical history, the optimal number of eggs needed for their own future family-building goals. Should it make sense for the donor, they may choose to pursue a second egg-sharing cycle to maximize the chances of success for everyone.
Matching with a donor in our frozen program can provide the opportunity to move forward with your family-building plans faster, as frozen eggs can be fertilized or shipped to your clinic immediately or as soon as the cycle is complete. Donors undergoing frozen cycles complete equally rigorous ovarian reserve testing. While the total number of frozen eggs available will vary based on the donor’s retrieval outcomes, every frozen match is guaranteed to have a minimum of at least 6 frozen eggs.
To learn more about these programs and the differences between them, click here.
How many embryos can I expect from an egg sharing round?
One 2015 study of 647 frozen donor eggs found that just three donor eggs would yield a little over one genetically normal embryo on average while nine donor eggs would be expected to yield three to four euploid embryos on average.

Keep in mind, these are just averages. Everyone’s experience is different and may be higher or lower than this.
Our Embryo Guarantee
While some agencies require you to pay extra to receive any form of a guarantee, Cofertility’s Embryo guarantee is built into our pricing.
This is our promise that if anything outside of your control prevents you from reaching the guaranteed minimum number of blastocyst-stage embryos for your match, we will rematch you at no additional charge until that minimum is met, up to three total matches
Read more about our Embryo Guarantee.
Cofertility - striving to be the best egg sharing program
We aim to be the best egg sharing program, providing an experience that honors, respects, and uplifts everyone involved. Here’s what sets us apart:
- Embryo guarantee. Our promise that if anything outside of your control prevents you from reaching the guaranteed minimum number of blastocyst-stage embryos for your match, we will rematch you at no additional charge until that minimum is met, up to three total matches.
- Donor empowerment. Our model empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
- Diversity: We’re proud about the fact that the donors on our platform are as diverse as the intended parents seeking to match with them. We work with intended parents to understand their own cultural values — including regional nuances — in hopes of finding them the perfect match.
- Human-centered. We didn’t like the status quo in egg donation. So we’re doing things differently, starting with our human-centered matching platform.
- Lifetime support: Historically, other egg donation options have treated egg donor matching as a one-and-done experience. Beyond matching, beyond a pregnancy, beyond a birth…we believe in supporting the donor-conceived family for life. Our resources and education provide intended parents with the guidance they need to raise happy, healthy kids and celebrate their origin stories.
We are obsessed with improving the family-building journey — today or in the future — and are in an endless pursuit to make these experiences more positive. Create a free account to get started today!
.png)
IVF after 40: Should I Use My Own Eggs or Donor Eggs?
For women who are in their 40s and considering IVF, a common question arises: should I use my own eggs or donor eggs? In this article, we’ll review valuable insights and information to help you make an informed decision on your IVF journey.
In recent years, advancements in reproductive technologies have given hope to many individuals and couples struggling with infertility. In vitro fertilization (IVF) in particular has enabled more people to become parents and grow their families. Some estimate that there have been over eight million babies born via IVF (including my own!). And 1 in 8 IVF cycles are estimated to involve eggs retrieved from a donor.
For women who are in their 40s and considering IVF, a common question arises: should I use my own eggs or donor eggs? In this article, we’ll review valuable insights and information to help you make an informed decision on your IVF journey.
How successful is IVF with your own eggs at 40?
Unfortunately, as we age our fertility naturally declines, and this decline becomes more significant after the age of 35. By the age of 40, a woman's ovarian reserve (the number and quality of eggs she has) is often diminished. Consequently, the success rates of IVF using a woman's own eggs decrease with age.
According to the Center for Disease Control (CDC) Assisted Reproductive Technology (ART) data, the live birth rate per IVF cycle for women over 40, using their own eggs, is 7.6%. This means that out of every 100 IVF cycles, only 7-8 result in a live birth.
While age plays a huge role in your chances of success, there are other factors that influence IVF outcomes including overall health, previous pregnancies, sperm health, the quality of the clinic, and the quality of the embryos. It is important to have realistic expectations when considering IVF with one's own eggs at the age of 40. A fertility doctor should be able to give you an idea of your chances of success with a proper fertility evaluation.
Should I try IVF with my own eggs or go straight to donor eggs?
Deciding whether to try IVF with your own eggs or proceed directly to donor eggs is a deeply personal and complex choice. Several factors should be taken into consideration, including your age, ovarian reserve, overall health, previous fertility history, and emotional readiness.
For those in their early 40s with a good ovarian reserve and no underlying fertility issues, attempting IVF with your own eggs may be a reasonable option. A fertility doctor can evaluate your specific circumstances and provide guidance based on their expertise.
On the other hand, some people want the fastest and most likely path to a healthy pregnancy and healthy baby. Especially if your journey has already been long, hard, and expensive, the decision to use donor eggs may bring renewed hope.
If your ovarian reserve is significantly diminished, or if previous attempts at IVF have been unsuccessful, using donor eggs may offer a higher chance of success. Donor eggs come from egg donors who have passed rigorous screening including ovarian reserve, reproductive health, general health, and genetics. This can increase the chances of achieving a successful pregnancy and live birth.
What is the success rate of IVF with donor eggs?
Donor egg IVF has the highest success rate of any fertility treatment. This means that donor eggs can drastically increase your chances of success! Around 53 percent of all donor egg cycles will result in at least one live birth. This percentage varies depending on the egg donor, recipient body mass index, stage of embryo at transfer, the number of oocytes retrieved, and the quality of the clinic.
At every age, the chances of birth with donor eggs is better, but those who benefit the most from donor eggs are women over 35 and those with low ovarian reserve. In fact, about one-quarter of women over 40 who succeeded with IVF did so through the use of donor eggs.

The chart was made using the SART Patient Predictor for an average woman (5’4”, 150 lbs) with diminished ovarian reserve. As you can see, the chances of live birth after one donor egg cycle is 54% for recipients under 40, and only goes down slightly after this.
What is the risk of miscarriage with donor eggs?
The short answer is that using donor eggs decreases the risk of miscarriage for most women. Especially for those who experienced previous miscarriages due to chromosomal abnormalities. Because egg donors are young (under 33) and medically cleared, outcomes with donor eggs are better than outcomes with a patient’s own eggs.
Age is a significant factor in miscarriage risk. As women age, the quality of their eggs decreases, and the risk of chromosomal abnormalities increases, which can lead to miscarriage. By using younger, healthier eggs from a donor, the risk of chromosomal abnormalities is significantly reduced.
Furthermore, the donor egg IVF process involves extensive screening of the donor to ensure that she is in good health and has a low risk of genetic disorders. This can further reduce the risk of miscarriage, as genetic disorders can be a significant contributor to pregnancy loss.
Pros and cons of using donor eggs vs. your own eggs
Let’s go over some of the advantages and disadvantages of using donor eggs for IVF.
The pros of using donor eggs include:
- Better egg quality: Eggs from donors tend to have better genetic quality, potentially reducing the risk of chromosomal abnormalities and genetic disorders.
- More embryos: A medically cleared egg donor is likely to lead to more embryos, often giving families more options, including gender selection.
- Increased success rates: Donor eggs come from young (under 33), healthy donors, which can improve the chances of successful fertilization, implantation, and pregnancy – getting a baby in your arms sooner.
The challenges of using donor eggs include:
- Emotional considerations: Using donor eggs may bring up complex emotional issues, such as feelings of loss, grief, or concerns about genetic connections. It is important to seek counseling or support to address these emotions.
- Financial costs: Using donor eggs adds an additional expense to the IVF process.
Find an amazing egg donor at Cofertility
At Cofertility, our program is unique. After meeting with hundreds of intended parents, egg donors, and donor-conceived people, we decided on an egg donation model that we think best serves everyone involved: egg sharing. We didn’t invent the concept of egg sharing, but we are the first to take it national (and even global!).
Here’s how it works: our unique model empowers women to take control of their own reproductive health while giving you the gift of a lifetime. Our donors aren’t doing it for cash – they keep half the eggs retrieved for their own future use, and donate half to your family.
We aim to be the best egg sharing program, providing an experience that honors, respects, and uplifts everyone involved. Here’s what sets us apart:
- Donor empowerment. Our model empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
- Diversity: We’re proud about the fact that the donors on our platform are as diverse as the intended parents seeking to match with them. We work with intended parents to understand their own cultural values — including regional nuances — in hopes of finding them the perfect match.
- Human-centered. We didn’t like the status quo in egg donation. So we’re doing things differently, starting with our human-centered matching platform.
- Lifetime support: Historically, other egg donation options have treated egg donor matching as a one-and-done experience. Beyond matching, beyond a pregnancy, beyond a birth…we believe in supporting the donor-conceived family for life. Our resources and education provide intended parents with the guidance they need to raise happy, healthy kids and celebrate their origin stories.
For those who match with a donor in our fresh egg donation program, the average number of mature eggs a family receives and fertilizes is 12. The number of eggs retrieved varies by patient and cycle, but can be predicted by a donor’s age, AMH, and antral follicle count, all of which will be known to you after the donor’s initial screening. Qualified candidates have an ample ovarian reserve for both their own needs and sharing. Egg share donors also often work closely with a fertility doctor to determine, based on their own medical history, the optimal number of eggs needed for their own future family-building goals. Should it make sense for the donor, they may choose to pursue a second egg-sharing cycle to maximize the chances of success for everyone.
Matching with a donor in our frozen program can provide the opportunity to move forward with your family-building plans faster, as frozen eggs can be fertilized or shipped to your clinic immediately. Donors undergoing frozen cycles complete equally rigorous ovarian reserve testing. While the total number of frozen eggs available will vary based on the donor’s retrieval outcomes, every frozen match is guaranteed to have a minimum of at least 6 frozen eggs.
To learn more about these programs and the differences between them, click here.
We are obsessed with improving the family-building journey — today or in the future — and are in an endless pursuit to make these experiences more positive. Create a free account to get started today!
How much do donor eggs cost?
The cost of egg sharing can vary based on whether you opt for a fresh or frozen donation cycle as well as other factors like the fertility clinic or donor's location. Unlike traditional egg donation, donors in egg sharing programs do not receive cash compensation, which can reduce your overall expenses.
For a more detailed breakdown of Cofertility's pricing, including estimates, you can visit our pricing page. All of our pricing also includes our Embryo Guarantee.
Summing it up
While IVF with one's own eggs can still offer a chance of success after 40, the use of donor eggs can significantly increase the chances of achieving a successful pregnancy and live birth.
Deciding between using your own eggs or donor eggs for IVF is a deeply personal choice that may be weighing on you. If you are hesitating to use donor eggs, we highly recommend connecting with a parent or support group of others who have walked down this path. We have never met a parent through egg donation who has regretted their decision. A fertility psychologist who has experience in this area can also provide guidance.
Ultimately, the goal is to make an informed choice that aligns with your desires, values, and the best chances of achieving a healthy pregnancy and fulfilling parenthood. Wherever you land, we wish you all the best.
Read more:
