egg bank

How to Use SART Data to Evaluate Fertility Clinics for Donor Egg IVF
Wondering how to evaluate fertility clinics for donor egg IVF? The SART database is a helpful place to start—but only if you know how to read between the lines. Here’s what to look for (and what to question).
When you’re pursuing egg donation to build your family, choosing the right fertility clinic can feel overwhelming. Everyone wants the best outcomes possible and while there’s no perfect formula for picking a clinic, the Society for Assisted Reproductive Technology (SART) database is one tool we have to evaluate IVF clinics.
SART collects detailed outcome data from hundreds of clinics across the U.S., reporting on everything from the number of cycles completed to live birth rates by patient age and treatment type. But understanding what the numbers mean and how to apply them to your unique family-building plans takes a bit of interpretation. For example, a clinic that reports higher live birth rates might simply be selecting patients with fewer fertility barriers, while another with more modest numbers could be working with harder-to-treat cases, including people with diminished ovarian reserve or complex medical histories.
This article walks through how to make sense of the SART Clinic Report, what success rates do (and don’t) tell you, and which filters are most relevant when you’re planning to use donor eggs. We’ll also cover red flags to watch for and other questions you should be asking alongside the data.
What SART data can tell you—and what it can’t
SART data is one of the most widely used sources for clinic success rates, as it reflects real outcomes, including pregnancies and live births after IVF. But it’s not a perfect apples-to-apples comparison tool. For starters, SART data is self-reported by clinics and reviewed for consistency, but not independently audited in full.
SART data also lags about two years behind, since it only includes cycles that have had time to result in a live birth. If you’re working with a newer clinic, they could be tracking and reporting outcomes to SART but just may not be reflected in the dataset quite yet.
The data is reported by cycle start, which includes any patient who initiated an IVF cycle, even if they didn’t proceed to egg retrieval or embryo transfer. That means reported live birth rates may include a denominator of patients who never got far enough for the treatment to have a real chance of success. Some clinics work hard to include every patient in their reported data; others may be more selective about who they treat, which can make their success rates appear higher.
Still, if you understand what you’re looking at, SART data can provide real insight, especially when you use filters and hone in on metrics that apply to your situation.
Looking up donor egg cycles in the SART report
To start, you can look up an IVF clinic by name or location here. If a clinic has multiple locations: they may have profiles associated with every location or they may only have profiles associated with their primary labs. The search functionality is also a bit sensitive; if you’re not locating a clinic by name, try searching by city or state.
When viewing a clinic’s report, you’ll see multiple sections, each focusing on different treatment types: cycles using a patient’s own eggs, cycles using donor eggs, and cycles using donated embryos. For intended parents working with an egg donor and possibly a gestational carrier, the donor egg data is most relevant.
Here’s what you’ll see in the donor egg section:
- Fresh donor egg cycles: These are cycles that involve using fresh donor eggs and a fresh embryo transfer.
- Frozen donor egg cycles: These are cycles that involve using frozen donor eggs and a fresh embryo transfer.
- Donor egg thawed embryos: These are cycles using frozen embryos (thawed before transfer) that were made with either fresh or frozen donor eggs.
- Donated embryos: These involve embryo transfers using embryos that were originally created by another individual or couple. These are all frozen embryo transfers.
Each of these comes with its own success rates, reported by age and often by the number of embryos transferred.
Understand the difference between a Fresh vs Frozen Embryo Transfer.
How to interpret success rates in the SART report
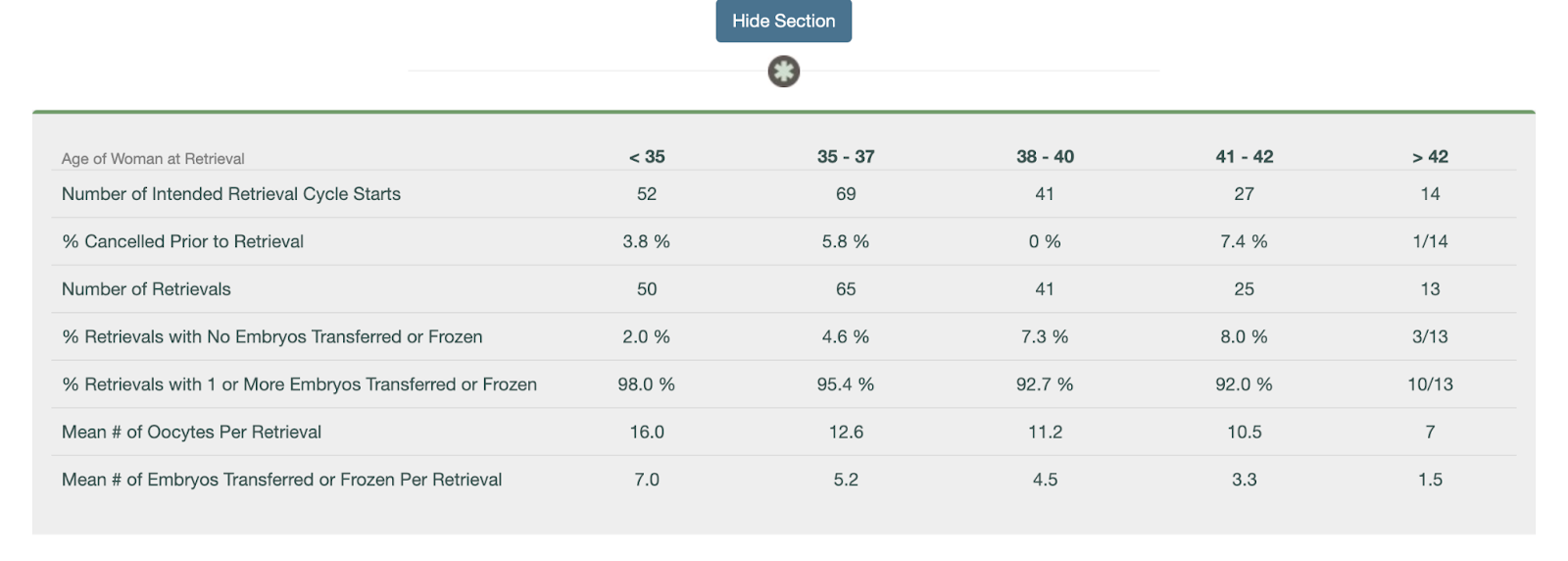
Once you’ve identified the donor egg section of a clinic’s SART report, you can start digging into the numbers. While the report doesn’t include every metric (like implantation rate), it does offer helpful data points to understand how often donor egg cycles result in live births—and how experienced the clinic is with this kind of care.
Here’s how to use the data:
- Look at the total number of embryo transfer procedures. This tells you how many donor egg transfers the clinic performed, which can give you a sense of their experience. A higher number means the clinic is regularly working with donor egg IVF families—an important signal if you’re pursuing this type of treatment.
- Check how many of those transfers resulted in live births. If there are fewer than 10 cycle starts in a category, live births are provided as a fraction. If there are 11 or more cycles, it’s provided as a percentage. While this isn’t a perfect metric, it offers a practical look at how effective the clinic is once a transfer occurs.
- Review singleton vs. multiple birth rates. A high singleton rate suggests the clinic emphasizes single embryo transfer (eSET), which is generally safer for both the carrier and the baby. High twin rates may boost reported pregnancy success but come with higher medical risks.
- If you’re using a gestational carrier (GC), ask the clinic for donor egg + GC outcomes. SART doesn’t break this out, but clinics should be able to provide this data. These cycles tend to be highly optimized and can reflect the clinic’s best-case outcomes.
While the SART report doesn’t show everything, it provides a meaningful snapshot of how well a clinic performs with donor egg cycles and how often they’re managing them. Combine this data with direct questions to the clinic to get a fuller picture of what you can expect.
Consider volume, but don’t assume more is always better
SART data shows how many cycles a clinic performs in a given year. Higher volume can indicate more experience and familiarity with a wide range of cases, but that doesn’t mean bigger is always better. A massive clinic might have shorter visit times, less personalized attention, or limited communication with physicians. Conversely, smaller clinics may offer more personalized care but might not have the same technological resources or lab investment.
Ask yourself what matters more to you: personalized attention and consistency, or access to a busy, highly specialized team? There’s no right answer—just what fits your preferences.
Don’t ignore what’s missing
Some clinics don’t report data to SART at all. While SART participation is voluntary, transparency should be a baseline expectation. If a clinic doesn’t report, ask why. It might be a red flag, or it might be an early-stage clinic without a full year of data yet.
It’s also worth noting that SART doesn’t report standalone success rates for thawed eggs (only fresh embryo transfers). So if you’re using frozen donor eggs—or if you’re planning to freeze embryos now and transfer later—those specific success rates won’t be visible. In those cases, ask the clinic directly about their outcomes from egg thaw cycles and embryo transfers using frozen material.
Be cautious about over-interpreting live birth per cycle
Clinics are incentivized to make their live birth per retrieval cycle look high, which can lead to some concerning practices like encouraging patients to transfer an embryo right away instead of banking multiple embryos for future family-building, or discouraging care for “poor responders” who may require multiple retrievals. These choices may boost reported rates but aren’t always in a patient’s best interest.
For intended parents hoping to have more than one child using the same donor, it may be smarter to focus on embryo banking before any transfer. But this approach - although strategic - can negatively impact the clinic’s live birth per cycle numbers. That’s why it's important to ask how your clinic approaches embryo banking and cumulative success planning.
Other questions to ask beyond the numbers
While SART data is valuable, it’s only one part of the clinic evaluation process. Consider also asking:
- What’s the average number of embryos your clinic transfers per cycle?
- How do you support intended parents using donor eggs or gestational carriers?
- What’s the experience like for people working with donor eggs?
You might also want to explore patient reviews on sites like FertilityIQ or attend a clinic info session to get a better feel for their values and communication style.
Bottom line
SART data can be a powerful tool when selecting a fertility clinic if you know how to use it wisely. Focus on donor egg cycles, apply relevant filters, and pay close attention to metrics like number of transfers, singleton birth rate, and outcomes per embryo transfer. Use the data to inform your questions, not as the only measure of quality.
Look for transparency, clarity, and a clinic that welcomes your questions. The right data can support your decision, but trust and care matter just as much.
If you work with Cofertility, we can help connect you with one of our many clinic partners.
Read more:

Whose Sperm Should We Use? How Gay Dads Can Decide What’s Fair
Deciding whose sperm to use can be an emotional and complex part of LGBTQ+ family building. Here's how gay dads can navigate fairness, biology, and shared parenthood.
For many gay male couples pursuing parenthood through assisted reproduction, one of the earliest and most personal decisions is whose sperm to use. It’s a question that can feel both logistical and loaded, because behind it are deep considerations about biology, identity, fairness, and family.
Some couples know from the start that one partner will be the biological parent, whether due to medical history, family planning goals, or personal preference. But for others, the answer isn’t so clear-cut. Many hope to give each partner the chance to have a biological connection to their child (or children). And with egg donation and gestational surrogacy, that possibility exists. The question is how to approach it.
A recent study published in F&S Reports (2025) sheds light on how male same-sex couples make these decisions and what challenges may arise along the way. Conducted through interviews with 20 gay dads and intended fathers, the study revealed four main drivers of decision-making: desire for genetic relatedness, perceived risk, desire for control, and cost. Here’s what Cofertility took away from the research—and how it can help guide your own thinking.
The case for using both partners’ sperm
Many couples choose to “split the eggs”—fertilizing donor eggs with sperm from each partner in the same IVF cycle. This allows both partners the chance to have a biological child, often with plans to transfer one embryo from each partner over time (e.g., one child biologically related to one dad, the next to the other).
This approach is sometimes called a “split cycle” or a “dual sperm source cycle.” It's seen as a way to balance biology, support equity in the relationship, and build a family where siblings share a genetic connection through the same egg donor.
In the study, one participant said, “We both wanted to be sperm sources because it was important for us to at least have one child from each of us.”
But while this can feel like the fairest option on paper, there are real-world considerations that can complicate things.
When fairness meets biology
Not every IVF cycle yields the same results for each partner. Some couples who split donor eggs found that one partner ended up with several viable embryos while the other had none. This can be disappointing, and in some cases, emotionally charged. One couple had to do an additional cycle after a poor outcome from the initial split, and it created tension.
“If we could have reversed time, it would probably have been better for just me to do the full eggs for fertilization, rather than splitting it in half,” one participant reflected.
Biological variability is outside anyone’s control, but it can feel personal when it plays out unequally within a relationship. This is why some couples ultimately choose to do separate cycles: one full cycle for each partner, either simultaneously or staggered over time. While more expensive, this option avoids embryo imbalances and may preserve a sense of fairness.
Choosing one partner's sperm
There are valid reasons couples might decide to use sperm from only one partner, at least initially. Common reasons include:
- One partner has a stronger reproductive profile (e.g., higher sperm count, younger age, better motility)
- One partner has a known genetic condition or family history
- The couple is prioritizing cost and wants to maximize outcomes with one fertilization cycle
- The couple already has a child biologically related to one partner and wants to continue with the same
- One partner cares deeply about having a biologically related child while the other does not
Sometimes the decision is more emotional than medical. One partner may have always dreamed of a biological child, while the other feels neutral. Or one may express a strong interest in being the biological parent of the first child, with openness to switching roles for a second.
There’s no wrong answer—what matters is that both partners feel heard.
Things to discuss before deciding
Whether you're leaning toward a dual sperm source cycle or not, here are a few questions to talk through together and with your clinic:
- Do we both want a biological connection to our children?
- What happens if one of us ends up with no viable embryos?
- Would we be open to doing more than one cycle if needed?
- If having more than one child, how important is it that our children share a genetic connection to each other?
- Are we aligned on what fairness looks like—for our relationship and future family?
These conversations can be emotional, and sometimes unexpected feelings come up. That’s normal. In fact, the study found that many couples wished they’d had more guidance upfront, especially when early expectations didn’t match the outcome.
Planning for siblings
Some couples choose an egg donor with the future in mind, hoping to create sibling embryos for each partner. Others want both kids to share the same donor, so they’re biologically related through their egg side, even if each child is biologically related to a different dad.
This is another reason why choosing and coordinating embryo creation in advance can be helpful. A shared cycle or two coordinated separate cycles can allow families to preserve embryos from both partners for use over time.
The role of cost—and how it shapes decisions
IVF with donor eggs and a gestational carrier is expensive—especially without insurance coverage. Many couples in the study shared that financial realities were the single biggest factor in how they planned their cycles.
Doing one shared IVF cycle is often more affordable than two separate ones. Some couples opted for a dual sperm source cycle even knowing that one partner might end up with fewer embryos, because it was their best shot financially.
Others made trade-offs on things like PGT-A testing, or even double embryo transfer (DET) in hopes of increasing efficiency—though each of these comes with its own implications.
At Cofertility, we understand that financial constraints shape real-life decisions. That’s why it’s so important to provide clear, honest information about options, trade-offs, and outcomes. Intended parents deserve tools and support—not just access.
A note on what’s “fair”
Fair doesn’t always mean equal. Fair might mean supporting the partner who feels strongly about having a genetic child, while the other feels fulfilled just being a parent. Fair might mean sharing biological parenthood over two children, or deciding together to prioritize what gives the highest odds of success now.
In the end, fairness in family building is about mutual respect, clear communication, and making decisions that honor both partners’ hopes, even when those hopes evolve over time.
If you’re navigating these questions now, know that you’re not alone—and you don’t have to figure it all out at once. What matters most is building the family that’s right for you. There’s more than one way to do that, and all of them start with intention.

Choosing an Egg Donor: The Role of Biomarkers
Choosing the right egg donor involves more than just age. Learn how fertility doctors use AMH, AFC, and age together to predict egg yield and guide your family-building decisions.
If you're pursuing egg donation to build your family, you’ve probably heard that age matters. However, when it comes to the number of eggs a donor might produce in a single cycle, age is only part of the picture. Fertility doctors use a combination of biological indicators called ovarian reserve markers to get a clearer sense of how a donor is likely to respond to stimulation medication. These markers include AMH (anti-Müllerian hormone), AFC (antral follicle count), and yes, age. Together, they can help predict how many eggs a donor might yield in a given cycle.
Understanding these biomarkers can help you make better decisions: whether that’s about which donor to match with, whether to split a cohort, or whether you may need multiple cycles to meet your family-building goals. This article explains what each of these markers means, how they’re used in donor screening, and what they can (and can’t) tell you about potential outcomes.
Donor AMH: anti-Müllerian hormone
AMH is a hormone released by cells in developing egg follicles. It gives a general sense of a person’s’s ovarian reserve, or the number of eggs they still have. In most people, AMH levels peak in the mid-20s. For intended parents working with an egg donor, a higher AMH level usually suggests the donor has a good chance of responding well to ovarian stimulation, meaning more eggs are retrieved in a single cycle.
That said, there’s a wide range of what’s considered “normal,” and AMH is just one piece of the puzzle. A very high AMH might raise the risk of ovarian hyperstimulation syndrome (OHSS), especially in donors with polycystic ovary syndrome (PCOS). While high AMH may seem appealing at first glance, it still needs to be considered within the broader clinical context. On the other hand, a lower AMH doesn’t necessarily mean a donor isn’t a good candidate, especially if they’re young and have a good antral follicle count.
At Cofertility, an AMH level of at least 2.0 ng/mL is required for our donors. This threshold is based on clinical data suggesting that donors with this level are more likely to have a strong response to fertility medications and produce enough eggs to support both donation and personal use.
AMH is measured through a simple blood test and is often one of the first screening tools used to assess a donor’s fertility potential.
Read more in Does AMH Matter When Choosing an Egg Donor?
Donor AFC: antral follicle count
Antral follicle count is a snapshot of how many follicles are visible on a donor’s ovaries at a particular point in their cycle, usually early in the menstrual cycle, when baseline testing is done. These are the small, fluid-filled sacs that each contain an immature egg. During a stimulation cycle, the follicles grow larger and the eggs inside them mature ,making them available for retrieval.
AFC is measured by transvaginal ultrasound, and it gives a real-time look at the ovaries. The more antral follicles, the higher the potential number of eggs that could be retrieved. In clinical terms, a “normal” AFC is typically somewhere between 10 and 20 follicles (counting both ovaries), but many donors exceed that.
AFC is considered one of the most reliable indicators of ovarian response. While AMH tells you about the pool of follicles available in a more general sense, AFC shows you what’s happening right now. Since AFC is a real-time snapshot of the ovaries, it can fluctuate slightly from month to month, but these variations are typically minor and don’t significantly impact how a donor is expected to respond. For intended parents, a donor with a strong AFC may provide reassurance that the stimulation cycle will likely yield a solid number of mature eggs.
Donor age: still an important piece of the puzzle
You already know age is a factor. But what’s important to understand is that age affects not just the number of eggs a donor may produce, but also the quality of those eggs—specifically, their likelihood of leading to a healthy embryo.
That’s why most egg donation programs set an age range for donors, usually between 21 and 33 years old (we follow these guidelines at Cofertility). While there’s no legal maximum age to become an egg donor, the American Society for Reproductive Medicine (ASRM) recommends that donors be under 34, and most clinics follow that guidance. Our limit accounts for the fact that it can take some time to match with intended parents and complete a cycle, and we want donors to still fall within the recommended age window by the time the cycle takes place.
Within that range, there can still be differences in both quantity and quality of eggs based on things beyond age.
That said, most donors who get medical clearance respond very well to stimulation and produce excellent-quality eggs, whether in their late 20s and early 30s. Age is just one variable, and when combined with the other biomarkers, it helps doctors build a fuller picture of what to expect from a cycle.
How these markers are used together
No single biomarker tells the whole story. Fertility doctors look at AMH, AFC, and age together to estimate a donor’s likely response to ovarian stimulation. This is sometimes called “ovarian reserve testing,” but the goal isn’t just to count eggs. It’s also to plan appropriately for stimulation protocols and optimize outcomes.
For example, if a donor has high AMH and high AFC, they might be expected to produce 20+ eggs in a cycle, and the care team may start with a lower dose of stimulation medications to reduce the risk of overstimulation. If another donor has AMH on the lower end of the normal range and an average AFC, the team may anticipate a more moderate yield (perhaps 10 to 15 eggs) and plan accordingly by using a higher starting dose of medications to optimize their response to treatment.
Limits of prediction
While AMH and AFC are helpful, they’re not crystal balls. A donor with stellar biomarkers could still have a retrieval cycle that yields fewer mature eggs than expected. Likewise, a donor with average numbers might surprise everyone with a strong response.
Biology isn’t always predictable, and cycle outcomes can vary even in the same donor across multiple cycles. That’s why experienced clinics combine biomarker data with close monitoring during the stimulation phase to make adjustments in real time.
It’s also worth noting that the number of eggs retrieved isn’t the only metric that matters. Fertilization rate, embryo development, and success rates with IVF transfer all depend on additional factors,some of which can’t be measured ahead of time.
What this means for you as an intended parent
As you look through donor profiles, you may see some numbers directly—such as AMH or age—or you might get a broader summary from your clinic about the donor’s reproductive potential. It’s a good idea to ask your doctor what these biomarkers might suggest about how many eggs the donor is likely to produce, and how that aligns with your goals.
That said, it’s important to understand that every donor listed has already cleared a rigorous screening process. Fewer than 5% of applicants are accepted into Cofertility’s egg sharing program. If a donor has made it through, it means our medical advisors (who are board-certified reproductive endocrinologists) have reviewed their health, biomarkers, and ovarian reserve, and determined if they’re likely to respond well to treatment.
Within this highly qualified group, small differences in biomarker levels may not translate to big differences in actual outcomes. Rather than fixating on a slightly higher AMH or AFC, it may be more helpful to focus on which donor feels like the right match for your family, whether that’s based on their background, values, personality, or something less tangible that just clicks for you.
The bottom line
AMH, AFC, and age can offer helpful insight into how many eggs a donor may produce and how your doctor will approach their care during the cycle. These biomarkers are useful tools for setting expectations and guiding decisions, but they’re not guarantees.
All egg donation involves some level of uncertainty, even with strong indicators. That’s why programs like Cofertility set high standards up front. This ensures that every donor in the pool has a solid chance of success. Once a donor is approved, the differences between candidates tend to narrow, and the best choice is often the one that feels most aligned with your values and goals—not just the numbers.
Ask questions, gather information, and talk with your care team. But don’t be afraid to trust your gut, too. The right match will meet both the medical criteria and feel like someone who could help you build the family you’ve been hoping for.
Read more:
- Why Egg Donor Age Matters (And Why It Doesn't)
- Does AMH Matter When Choosing an Egg Donor?
- Will My Baby Look Like Me If I Use an Egg Donor?
- Shared vs. Separate Egg Donor Cycles: A Guide for Gay Dads

Cofertility’s Fresh Vs. Frozen Egg Donation Program: Which is Right for Me?
If you’re embarking on the donor egg IVF journey as an intended parent, one of the first decisions you'll face is whether to do a fresh or frozen egg donation cycle. At Cofertility, we offer both options, each with its own unique advantages.
If you’re embarking on the donor egg IVF journey as an intended parent, one of the first decisions you'll face is whether to do a fresh or frozen egg donation cycle. At Cofertility, we offer both options, each with its own unique advantages. But before we dive into the specifics of our fresh and frozen egg donation programs, it's important to highlight a few key aspects of the Cofertility model and experience that remain constant, regardless of which path you choose.
First and foremost, every donor at Cofertility participates in our unique egg sharing model. Instead of receiving cash compensation, Cofertility donors complete a split cycle in which they keep half of the mature eggs retrieved, and donate the other half to intended parents. This means that our donors aren't motivated by financial compensation, but rather by the opportunity to help your family today alongside their own future family building goals. It's a win-win situation that ensures our donors are genuinely committed to the process and aligns their interests with those of intended parents.
Secondly, no matter which program you opt for, you'll be protected by our Embryo Guarantee. While the scope of the guarantee varies with our fresh versus frozen donation programs, know that everyone on our team is deeply committed to helping you achieve your dream of parenthood, and this guarantee reflects that commitment.
Third, regardless of the program you choose, you’ll have the option to decide between having a disclosed or undisclosed relationship with the egg donor. You can also meet with the donor in either program, though the timing of that meeting varies based on whether you go fresh or frozen.
With these promises in place, let's explore the specific features of our fresh and frozen programs to help you determine which path might be the best fit for your family-building journey.
Cofertility’s frozen egg donation program
Matching with a donor in our frozen egg donation program offers several benefits that make it an attractive option for many intended parents.
Increased certainty
A significant advantage of matching with a donor in our frozen program is the increased certainty it brings to the egg donation process. When you match with a donor in our frozen program, she will have already completed her initial retrieval. With things like genetic testing results and psych clearance in hand, this means fewer unknowns and a smoother path forward.
But what does this mean for you in practical terms? It means less waiting, less anxiety, and more confidence in the process. You'll know from the start that your chosen donor has met all medical requirements to donate, reducing the risk of last-minute surprises or disappointments. This can be particularly reassuring for intended parents who have experienced setbacks in their fertility journey and are seeking a more predictable path forward.
Speed
If time is of the essence in your family-building journey, matching with donors participating in our frozen program might be a great fit. Since the time-consuming screening process is complete, the period from matching to embryo creation can be significantly shorter. This is particularly beneficial if you're eager to transfer embryos as soon as possible.
With a fresh egg donation cycle, you might wait one to three months for your donor to complete all necessary screenings and synchronize her cycle with yours. When you match with a donor in our frozen program, you could potentially be ready to create embryos within days of matching. For many intended parents, especially those who feel that time is of the essence, this acceleration of the process can be a game-changer.
Fixed cost transparency
Matching with a donor in our frozen program comes with a clearly defined fixed cost. This includes all expenses related to the donor’s retrieval and screening. Because the cycle has already been completed, you’ll know exactly what you're committing to. This predictability simplifies financial planning and lets you move forward fully informed about the costs involved.
Cofertility’s fresh egg donation program
Matching with a donor from our fresh egg donation program also has its own unique benefits that many intended parents find appealing.
Fresh egg embryo creation
One of the primary advantages of fresh egg donation is the ability to create embryos immediately upon egg retrieval. Some doctors prefer to fertilize fresh eggs vs. previously frozen eggs. This is because it could potentially lead to a higher number of healthy embryos, as it eliminates the need for egg thawing, a process that can sometimes result in the loss of some eggs.
Every egg is precious in this process. So while freezing techniques have advanced significantly in recent years, with vitrification there's still a small chance that some eggs may not survive the thawing process. With fresh eggs, you're working with eggs in their most viable state, potentially increasing your chances of creating healthy embryos.
Local cycles and continuity of care
When you match with a donor from our fresh egg donation program, you have the option of having that donor cycle at your clinic under the care of your own doctor. If you've already established a strong relationship with your fertility team, this ensures continuity throughout the entire process, from egg retrieval to embryo transfer.
This continuity can be incredibly valuable. Your fertility team already knows your medical history, understands your specific situation, and has likely built a rapport with you. Being able to continue working with them through the egg donation process can provide an added layer of comfort and familiarity during what can be an emotionally charged time.
Additionally, having the egg retrieval performed at your local clinic means you have more control over the process. You can be present (if you choose) on the day of the retrieval, adding to the sense of involvement and connection to the process.
A chance to meet the donor before the match is official
With either program, you’ll have the option of having a disclosed or undisclosed donation and can choose to meet the donor if that’s something both parties are interested in.
However, if you’re interested in matching with a donor from our fresh program, you’ll have the unique opportunity to potentially meet with the donor before she begins her cycle as part of our mutual matching process. This can be a meaningful experience for intended parents who value this personal connection from the outset.
For some intended parents, meeting the donor before the retrieval can help solidify their choice and create a sense of connection to the process. It can be an opportunity to express gratitude, ask questions, or simply put a face to the generous individual who is helping to make your dreams of parenthood a reality.
It's important to note, however, that this meeting is entirely optional. We understand that every intended parent and egg donor has different comfort levels when it comes to donor contact, and we respect whatever level of interaction you prefer.
Making your decision: it's all about finding your perfect match
Ultimately, for many intended parents, the choice between our fresh and frozen programs often comes down to finding the right donor. Both programs have their merits, and the best choice for you will depend on your specific circumstances, preferences, and the connection you feel with potential donors.
If you're open to either journey, we recommend exploring both options. You might find that you connect deeply with a donor in our fresh egg donation program, or you might discover that the perfect donor for you has already completed her cycle as a part of our frozen egg donation program.
Consider your priorities:
- Is time a critical factor for you? If so, frozen egg donation might be your best bet.
- Do you feel strongly about using fresh eggs? Then fresh egg donation could be the way to go.
- Is the ability to meet your donor before the retrieval important to you? With donors in our fresh egg donation program, you could have this opportunity.
- Regardless of which path you choose, all Cofertility intended parents are covered by our Embryo Guarantee.
At Cofertility, we're committed to supporting you through every step of your journey, regardless of which program you choose. Our team is here to answer your questions, address your concerns, and help you navigate this important decision.
Remember, this is your journey. Trust your instincts, ask questions, and don't hesitate to reach out to our team for guidance. We're here to help you navigate these decisions and find the path that feels right for you.
In the end, whether you go fresh or frozen, what matters most is the family you're building and the love that will fill your home. That is the most beautiful outcome of all. Your future child won't care whether they came from fresh or frozen eggs – they'll just be thrilled to be part of your family.
So take a deep breath, trust in the process, and know that with Cofertility by your side, you're one step closer to holding your baby in your arms. We’ve got hundreds of incredible donors on our egg donation platform who would love to help you make your dreams of parenthood a reality.
.png)
Which Should I Find First: An Egg Donor or a Surrogate?
The order in which you find a surrogate or egg donor will depend on your individual circumstances and needs. In this guide, we’ll go over a few things to consider.
If you are considering using a surrogate and an egg donor to help you start or grow your family, the order in which you find a surrogate or egg donor will depend on your individual circumstances and needs. In this guide, we’ll go over a few things to consider when deciding whether to find a surrogate or an egg donor first.
Surrogacy vs. egg donation
Surrogacy is a process in which a woman carries and delivers a child for someone else. If you are considering using a gestational carrier (aka surrogate), you will likely need to work with an agency to help match with someone who has been pre-qualified to carry your child. You will also need to work through the legal and medical aspects of surrogacy, including the surrogacy agreement and the medical screening and evaluation process.
An egg donor is a woman who donates her eggs to another person or couple. If you are considering using an egg donor, you will need to match with an egg donor who is willing to donate her eggs to you. You will also need to consider the medical and legal aspects of using an egg donor, including the egg donor agreement and the medical screening, evaluation, and retrieval process.
Who would need both a surrogate and egg donor?
There are lots of cases where families need both a gestational carrier and egg donor to have a child. Here are a few examples:
- Infertility: Some individuals or couples may be unable to conceive or carry a pregnancy to term due to infertility. In these cases, they may consider using both a surrogate and an egg donor to help them increase their chances of having a child.
- Single individuals: Some single individuals, especially those born male, may consider using a surrogate and an egg donor, along with their own sperm or donor sperm, to help them become parents.
- LGBTQ+ couples: Some same-sex couples may consider using a surrogate and an egg donor to help them become parents. For example, a gay male couple may use a surrogate and an egg donor to carry and give birth to a child that is genetically related to one of the men.
- Medical conditions: Some individuals or couples may have medical conditions that prevent them from getting pregnant, undergoing IVF, and/or carrying a pregnancy to term. In these cases, they may consider using both a surrogate to carry their child for them.
So which comes first, egg donor or surrogate?
In most cases, we recommend starting by matching with an egg donor. Many surrogacy agencies cannot sign up families who do not yet have healthy embryos to transfer. This is because gestational carriers are in high demand and they don’t want to wait months after matching in order to start the transfer process. On the other hand, once you have embryos made through donor eggs, those can be frozen and used at any point in the future.
You could also begin the search for a gestational carrier and an egg donor at the same time, knowing that the waitlist for a gestational carrier is far longer than the process to get donor eggs.
How long does it take to match with an egg donor?
The timeline can vary, but in total the process from match to cycle with Cofertility is generally be two to four months. Once you create a free account, you’ll gain access to our matching platform and can start to learn more about our donors. After you match with a Split member (who will be freezing her eggs and donating half to your family), we begin the process of scheduling her screening and testing with your clinic, which generally takes a few weeks. Once your doctor gives the go-ahead, we’d set a date for the cycle at a time that is mutually convenient.
You may decide to fertilize the embryos as soon as the eggs are retrieved or you can freeze the eggs and thaw them to be fertilized at a later date. If you do create embryos at the time of retrieval, they can be frozen in storage until you match with a surrogate or are ready to move forward with the transfer.
How long does it take to match with a surrogate?
The process of matching with a surrogate varies in length and may depend on a variety of factors, including the location and availability of surrogates, the intended parents' preferences and requirements, and the legal and medical requirements involved in the surrogacy process based on your state. In general, the process of finding a surrogate may take several months to a year.
Learn more
Ultimately, the decision of whether to find a surrogate or an egg donor first will depend on your individual circumstances and needs. It may be helpful to speak with your doctor to determine the best course of action for your situation.
Cofertility is a human-first fertility ecosystem rewriting the egg donation experience. Our Family by Co platform serves as a more transparent, ethical egg donor matching platform. Create a free account today!
.png)
Six Reasons Why Egg Sharing is an Ideal Egg Donation Model for Intended Parents
In traditional egg donation, the donor's eggs are given to the intended parents in exchange for cash compensation. However, in the increasingly popular egg sharing model, the donor has the opportunity to keep half of the eggs retrieved for her own future family planning. At Cofertility, we exclusively work under the egg sharing model, which we call Split, because we think it’s ideal for everyone involved – the intended parents, the egg donor, and ultimately the donor-conceived child.
In traditional egg donation, the donor's eggs are given to the intended parents in exchange for cash compensation. However, in the increasingly popular egg sharing model, the donor has the opportunity to keep half of the eggs retrieved for her own future family planning.
At Cofertility, we exclusively work under the egg sharing model, which we call Split, because we think it’s beneficial for everyone involved – the intended parents, the egg donor, and ultimately the donor-conceived child. In this article, we will explore six reasons why we think egg sharing is a compelling model for egg donation, focusing on benefits such as increased donor commitment, the absence of financial implications, and a more diverse pool of potential donors.
1. Donors have a personal stake in the outcomes, increasing donor commitment
One significant benefit of the egg sharing model is that donors have a personal stake in the outcomes. When donors contribute a portion of their eggs in exchange for their own IVF treatment down the line, they are invested not only in helping intended parents but also in achieving their own fertility goals. This shared interest leads to a greater sense of commitment and dedication from the donors, potentially resulting in higher-quality eggs and improved success rates.
2. Cash compensation models can lead some egg donors to conceal relevant medical information
The American Society for Reproductive Medicine (ASRM) published specific guidance regarding egg donor compensation in 2021. In this guidance, they acknowledge that excessive monetary compensation could create the possibility of undue inducement and exploitation of egg donors.
The guidance points out, “Women may agree to provide oocytes based on their financial need. High levels of compensation also could lead some prospective donors to conceal medical information relevant to their own health or that of their genetic offspring in order to be more likely to be selected for oocyte donation.”
However, in the egg sharing model, where the focus is on shared outcomes rather than financial gain, donors may be more likely to disclose any pertinent medical information, ensuring the best possible match and reducing the risk of undisclosed medical issues that may impact the intended parents or the resulting child's well-being.
3. Most donor-conceived people feel the exchange of money for donor eggs is wrong
In the context of egg sharing, compensation is not based on financial transactions. Instead, it focuses on the shared goal of success for both parties. This approach eliminates the potential discomfort and ickiness often associated with cash compensation, and avoids the perception of treating eggs as commodities.
A 2021 Harvard study found that 62% of donor-conceived adults felt the exchange of money for donor gametes was wrong, and 41% were troubled by the fact that money was exchanged around their conception. This is why we created our Split program. This unique model empowers women to take control of their own reproductive health while giving you the gift of a lifetime. Our donors aren’t doing it for cash – they keep half the eggs retrieved for their own future use, and donate half to your family.
By removing financial incentives, the process feels meaningful and preserves the dignity of all parties involved.
4. We’re able to recruit a more diverse pool of donors
Our model not only empowers our donors by giving them control over their own fertility, but it also enables us to recruit a truly exceptional group of donors. Our donors are motivated by the opportunity to help others start their families while also taking charge of their own reproductive futures. By offering this unique Split model, we have been able to attract a diverse and talented group of women who are passionate about helping others and committed to making a difference in the world.
5. Donors get to proactively invest in their own reproductive future
Egg sharing allows donors to actively invest in their own reproductive future while helping intended parents fulfill their dreams of having a child. By keeping half of the eggs retrieved, egg donors are proactively taking steps to preserve their fertility options and increase their chances of successful pregnancies in the future. This dual benefit of participating in the egg sharing model enables donors to make a meaningful investment in their own reproductive health, while simultaneously providing hope and support to intended parents who are seeking to build their families. It empowers donors to take control of their reproductive journey and make decisions that align with their long-term family planning goals.
6. Donors are happy with their decision
One compelling reason to consider egg sharing is the high level of donor satisfaction and positive experiences reported by individuals who have participated in this model. According to one study, the vast majority of egg share donors are happy with their decision. In fact, a significant majority of egg share donors, 83.3%, said they would even donate again.
This statistic reflects the positive impact and personal fulfillment donors experience through their participation in the egg sharing process. Only 2.1% regret their decision, underscoring the fact that the decision to participate in egg sharing is often met with a sense of satisfaction, knowing that their contribution has made a meaningful difference in someone else's life. The positive feedback from donors highlights the mutually beneficial nature of the egg sharing model, reinforcing the notion that it can be a rewarding and fulfilling experience for all parties involved.
Cofertility - striving to be the best egg sharing program
We aim to be the best egg sharing program, providing an experience that honors, respects, and uplifts everyone involved. Here’s what sets us apart:
- Donor empowerment: Our model empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
- Diversity: We’re proud about the fact that the donors on our platform are as diverse as the intended parents seeking to match with them. We work with intended parents to understand their own cultural values — including regional nuances — in hopes of finding them the perfect match.
- Human-centered: We didn’t like the status quo in egg donation. So we’re doing things differently, starting with our human-centered matching platform.
- Embryo Guarantee: We’re committed to helping your family grow, and proud to offer a generous Embryo Guarantee to every intended parent we work with.
- Lifetime support: Historically, other egg donation options have treated egg donor matching as a one-and-done experience. Beyond matching, beyond a pregnancy, beyond a birth…we believe in supporting the donor-conceived family for life. Our resources and education provide intended parents with the guidance they need to raise happy, healthy kids and celebrate their origin stories.
We are obsessed with improving the family-building journey — today or in the future — and are in an endless pursuit to make these experiences more positive. Create a free account to get started today!
