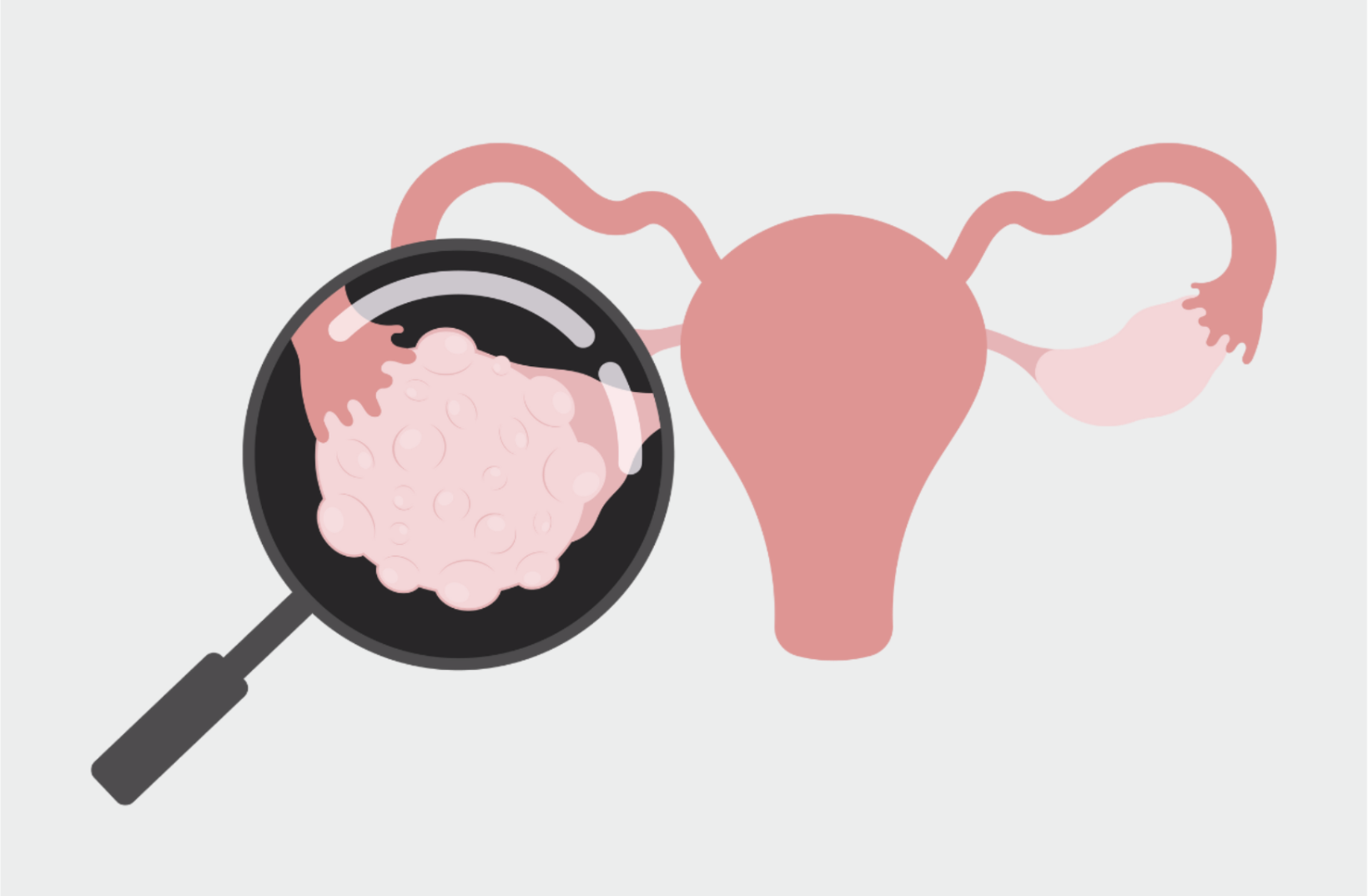
Egg freezing is an empowering option for family planning, but sometimes ovarian cysts can throw a wrench in the timing or progression of a cycle. Ovarian cysts are common and usually benign, yet their presence can influence how your body responds to ovarian stimulation, how many follicles develop, and even the egg retrieval process.
In this article, we’ll explain what ovarian cysts are, highlight the types most relevant to fertility (functional cysts, endometriomas, and dermoid cysts), and discuss how each type might delay or impact an egg freezing cycle.
What are ovarian cysts?
Ovarian cysts are fluid-filled sacs or pockets that develop within or on the surface of an ovary. They can occur in women of all ages and are often discovered during routine pelvic ultrasounds, including the baseline ultrasound that precedes an egg freezing cycle. The good news is that most ovarian cysts are benign (non-cancerous) and many are even a normal part of the menstrual cycle.
For example, every month, a follicle (which appears as a small cyst on ultrasound) grows to release an egg at ovulation; afterward, that follicle develops into a corpus luteum, a cyst-like structure that produces hormones. These are called functional cysts, and under normal conditions, they resolve on their own. Cysts vary in size and type. Small cysts often cause no symptoms, while larger ones can sometimes cause bloating, pelvic discomfort, or menstrual cycle irregularities.
In the context of egg freezing or donation, cysts are quite commonly seen – either as part of the intended ovarian stimulation (growing multiple follicles that look like cysts on the ovary) or as unexpected cysts present before stimulation begins.
It’s usually the unexpected, “abnormal” cysts that may need management. Key factors are the cyst’s type, size, and whether it produces hormones. Depending on those factors, a cyst can be simply observed over time, treated with medication, drained, or surgically removed.
Types of cysts that can affect egg freezing
Functional cysts
As shared above, functional cysts are the most common. These include follicular cysts (which form when a follicle doesn’t release its egg) and corpus luteum cysts (which can form after ovulation). These are usually temporary and often resolve on their own within a few weeks or with a short course of birth control pills. But if a functional cyst is present at your baseline ultrasound and is producing hormones like estrogen or progesterone, it could throw off your hormone levels and interfere with proper follicle development. In those cases, your doctor might delay the cycle until the cyst clears.
Dermoid cysts
Dermoid cysts (also called teratomas) are benign growths that often contain a mix of tissue types, like hair or skin. They don’t produce hormones and are not typically associated with impaired egg quality. However, large dermoids can take up space in the ovary or increase the risk of ovarian torsion during stimulation. Research shows that ovaries with dermoid cysts—or with a history of dermoid removal—tend to have fewer follicles than the unaffected ovary, with about a 40% reduction on average. Open surgery may reduce ovarian reserve more than minimally invasive approaches like laparoscopy. Still, studies have found no significant differences in IVF outcomes such as eggs retrieved or pregnancy rates. Most of the time, small dermoids don’t interfere with egg freezing, and many doctors recommend freezing eggs first and addressing the cyst later if needed.
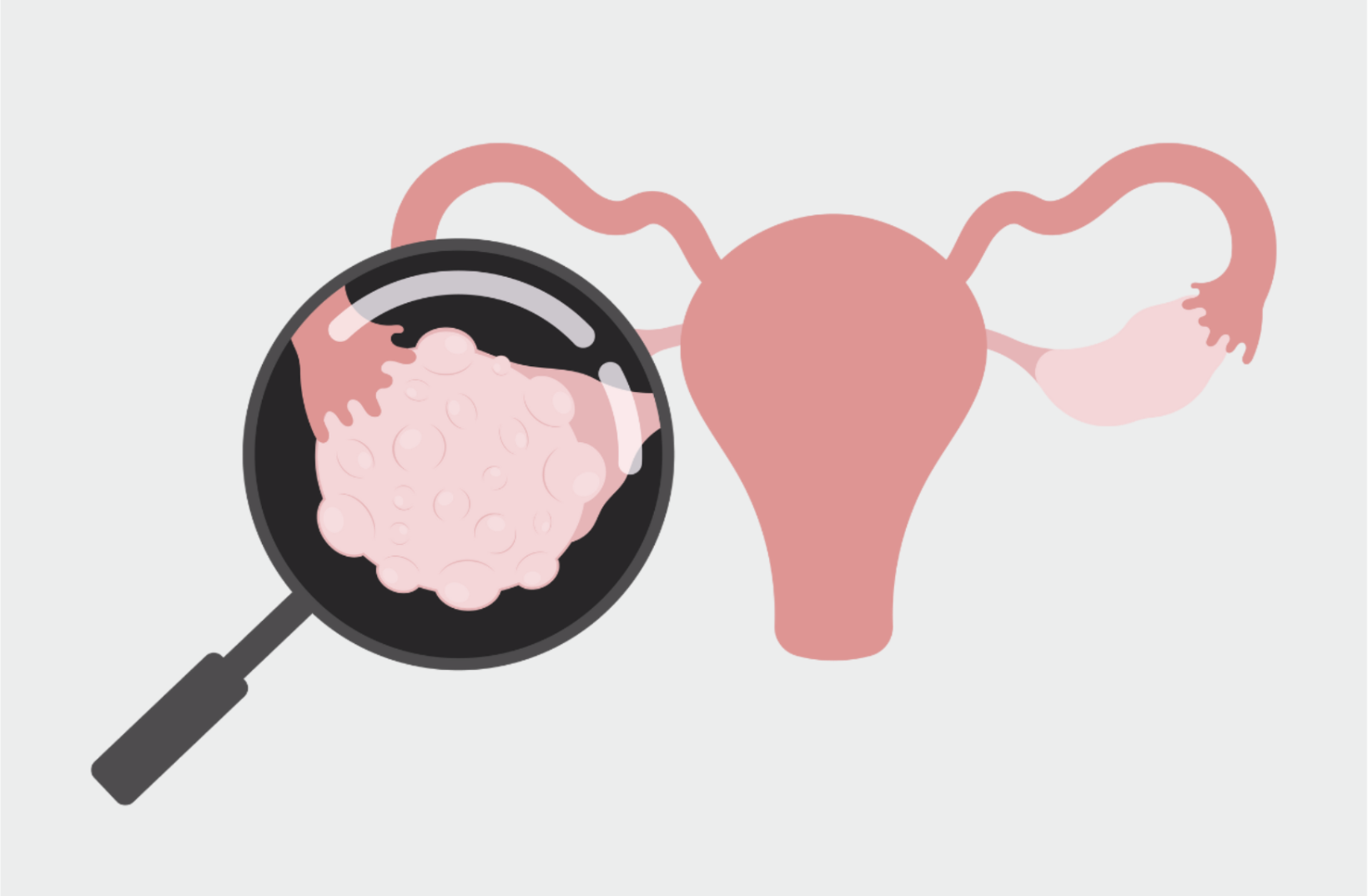
Endometriomas
Endometriomas are cysts caused by endometriosis, a condition where tissue similar to the uterine lining grows outside the uterus. According to a meta analysis of nine published studies, these cysts can damage ovarian tissue, reduce ovarian reserve, and create an inflammatory environment that might impact egg quality. They can also make retrieval more technically challenging. Depending on the size and symptoms, your doctor may recommend moving forward with egg freezing before having surgery to remove an endometrioma, since the surgery itself can reduce egg count.
Cystadenomas
Cystadenomas are benign growths that develop on the surface of the ovary and can be filled with either a watery fluid (serous cystadenomas) or a thicker, mucous-like substance (mucinous cystadenomas). While they are typically non-cancerous, they can grow large and take up space within the ovary, which may impact the number of follicles that can develop during stimulation. Depending on size and symptoms, your doctor may recommend monitoring or surgical removal—usually after completing egg freezing.
Ovarian cancer
Ovarian cancer is rare in people undergoing egg freezing, especially in younger age groups. However, if a cyst has suspicious features on ultrasound, your doctor may order additional imaging or tumor marker tests to rule out malignancy. If there’s any concern, your cycle may be delayed until further evaluation is complete. Malignant ovarian cysts require a different treatment path, and fertility preservation planning would need to be closely coordinated with an oncologist.
How cysts can impact your egg freezing cycle
Cycle delays
The most common impact of a cyst is a delay in starting your egg freezing cycle. If a cyst is producing hormones, your doctor might wait until your hormone levels normalize before beginning stimulation. This is typically just a short postponement, often one menstrual cycle or less.
Hormonal interference
Cysts that secrete estrogen or progesterone can disrupt the hormonal baseline necessary to begin a successful cycle. Your fertility doctor may choose to monitor the cyst or prescribe birth control to suppress ovarian activity until hormone levels return to the ideal range.
Fewer eggs or more complex retrievals
If a cyst is taking up space in the ovary, there may be fewer follicles able to grow on that side. Inflammatory cysts like endometriomas can also compromise egg quality. Some cysts, depending on their location and size, can make the egg retrieval procedure a bit more complex, but fertility doctors are trained to manage these situations safely.
Cyst management is individualized
In most cases, a cyst won’t ruin your egg freezing cycle—but it might delay it or reduce the number of eggs retrieved from one ovary. Your doctor will take into account your ovarian reserve, hormone levels, and any symptoms you’re having. If treatment or surgery is needed, you can make a plan together about when to proceed with egg freezing.
The bottom line
Cysts are common, and most won’t derail your fertility plans. In some cases, they may delay your cycle or slightly lower your egg count—but with good monitoring and a proactive plan, you can still have a successful egg freezing experience. If your clinic spots a cyst on your baseline ultrasound, they’ll talk you through next steps based on its type, size, and impact. You’re not alone in this—your care team is equipped to navigate cysts while helping you reach your egg freezing goals.