fertility testing

How to Use SART Data to Evaluate Fertility Clinics for Donor Egg IVF
Wondering how to evaluate fertility clinics for donor egg IVF? The SART database is a helpful place to start—but only if you know how to read between the lines. Here’s what to look for (and what to question).
When you’re pursuing egg donation to build your family, choosing the right fertility clinic can feel overwhelming. Everyone wants the best outcomes possible and while there’s no perfect formula for picking a clinic, the Society for Assisted Reproductive Technology (SART) database is one tool we have to evaluate IVF clinics.
SART collects detailed outcome data from hundreds of clinics across the U.S., reporting on everything from the number of cycles completed to live birth rates by patient age and treatment type. But understanding what the numbers mean and how to apply them to your unique family-building plans takes a bit of interpretation. For example, a clinic that reports higher live birth rates might simply be selecting patients with fewer fertility barriers, while another with more modest numbers could be working with harder-to-treat cases, including people with diminished ovarian reserve or complex medical histories.
This article walks through how to make sense of the SART Clinic Report, what success rates do (and don’t) tell you, and which filters are most relevant when you’re planning to use donor eggs. We’ll also cover red flags to watch for and other questions you should be asking alongside the data.
What SART data can tell you—and what it can’t
SART data is one of the most widely used sources for clinic success rates, as it reflects real outcomes, including pregnancies and live births after IVF. But it’s not a perfect apples-to-apples comparison tool. For starters, SART data is self-reported by clinics and reviewed for consistency, but not independently audited in full.
SART data also lags about two years behind, since it only includes cycles that have had time to result in a live birth. If you’re working with a newer clinic, they could be tracking and reporting outcomes to SART but just may not be reflected in the dataset quite yet.
The data is reported by cycle start, which includes any patient who initiated an IVF cycle, even if they didn’t proceed to egg retrieval or embryo transfer. That means reported live birth rates may include a denominator of patients who never got far enough for the treatment to have a real chance of success. Some clinics work hard to include every patient in their reported data; others may be more selective about who they treat, which can make their success rates appear higher.
Still, if you understand what you’re looking at, SART data can provide real insight, especially when you use filters and hone in on metrics that apply to your situation.
Looking up donor egg cycles in the SART report
To start, you can look up an IVF clinic by name or location here. If a clinic has multiple locations: they may have profiles associated with every location or they may only have profiles associated with their primary labs. The search functionality is also a bit sensitive; if you’re not locating a clinic by name, try searching by city or state.
When viewing a clinic’s report, you’ll see multiple sections, each focusing on different treatment types: cycles using a patient’s own eggs, cycles using donor eggs, and cycles using donated embryos. For intended parents working with an egg donor and possibly a gestational carrier, the donor egg data is most relevant.
Here’s what you’ll see in the donor egg section:
- Fresh donor egg cycles: These are cycles that involve using fresh donor eggs and a fresh embryo transfer.
- Frozen donor egg cycles: These are cycles that involve using frozen donor eggs and a fresh embryo transfer.
- Donor egg thawed embryos: These are cycles using frozen embryos (thawed before transfer) that were made with either fresh or frozen donor eggs.
- Donated embryos: These involve embryo transfers using embryos that were originally created by another individual or couple. These are all frozen embryo transfers.
Each of these comes with its own success rates, reported by age and often by the number of embryos transferred.
Understand the difference between a Fresh vs Frozen Embryo Transfer.
How to interpret success rates in the SART report
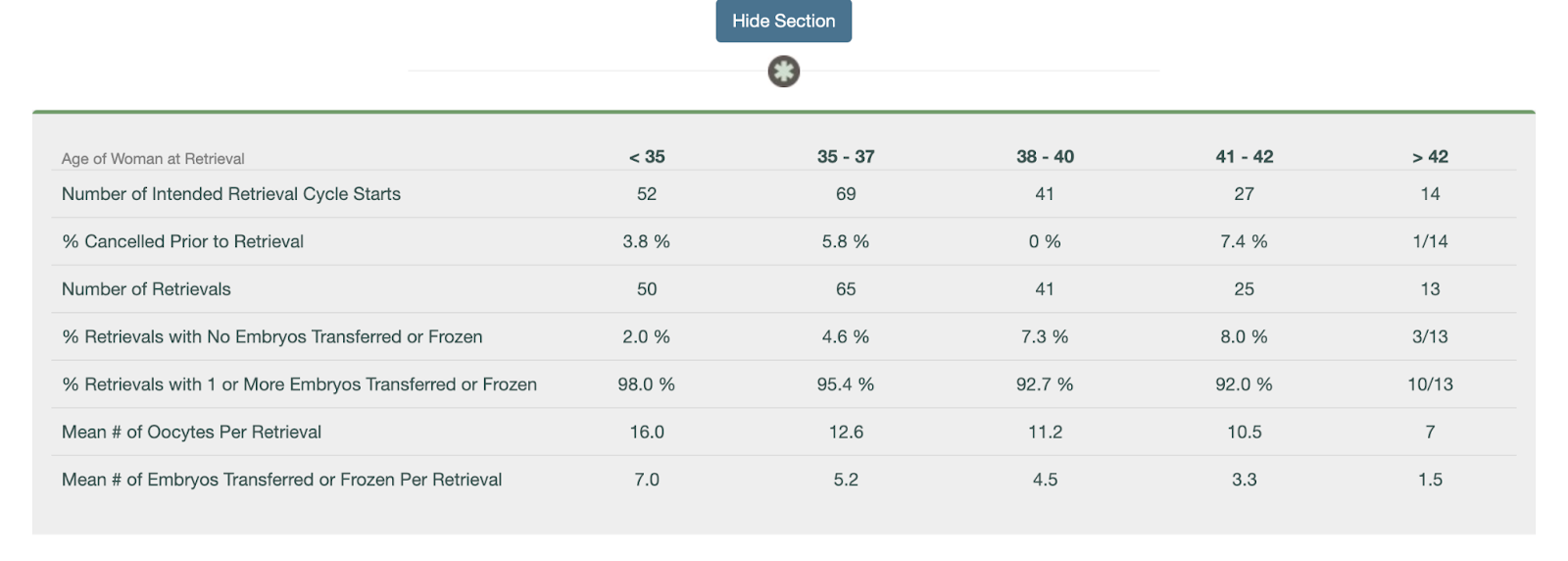
Once you’ve identified the donor egg section of a clinic’s SART report, you can start digging into the numbers. While the report doesn’t include every metric (like implantation rate), it does offer helpful data points to understand how often donor egg cycles result in live births—and how experienced the clinic is with this kind of care.
Here’s how to use the data:
- Look at the total number of embryo transfer procedures. This tells you how many donor egg transfers the clinic performed, which can give you a sense of their experience. A higher number means the clinic is regularly working with donor egg IVF families—an important signal if you’re pursuing this type of treatment.
- Check how many of those transfers resulted in live births. If there are fewer than 10 cycle starts in a category, live births are provided as a fraction. If there are 11 or more cycles, it’s provided as a percentage. While this isn’t a perfect metric, it offers a practical look at how effective the clinic is once a transfer occurs.
- Review singleton vs. multiple birth rates. A high singleton rate suggests the clinic emphasizes single embryo transfer (eSET), which is generally safer for both the carrier and the baby. High twin rates may boost reported pregnancy success but come with higher medical risks.
- If you’re using a gestational carrier (GC), ask the clinic for donor egg + GC outcomes. SART doesn’t break this out, but clinics should be able to provide this data. These cycles tend to be highly optimized and can reflect the clinic’s best-case outcomes.
While the SART report doesn’t show everything, it provides a meaningful snapshot of how well a clinic performs with donor egg cycles and how often they’re managing them. Combine this data with direct questions to the clinic to get a fuller picture of what you can expect.
Consider volume, but don’t assume more is always better
SART data shows how many cycles a clinic performs in a given year. Higher volume can indicate more experience and familiarity with a wide range of cases, but that doesn’t mean bigger is always better. A massive clinic might have shorter visit times, less personalized attention, or limited communication with physicians. Conversely, smaller clinics may offer more personalized care but might not have the same technological resources or lab investment.
Ask yourself what matters more to you: personalized attention and consistency, or access to a busy, highly specialized team? There’s no right answer—just what fits your preferences.
Don’t ignore what’s missing
Some clinics don’t report data to SART at all. While SART participation is voluntary, transparency should be a baseline expectation. If a clinic doesn’t report, ask why. It might be a red flag, or it might be an early-stage clinic without a full year of data yet.
It’s also worth noting that SART doesn’t report standalone success rates for thawed eggs (only fresh embryo transfers). So if you’re using frozen donor eggs—or if you’re planning to freeze embryos now and transfer later—those specific success rates won’t be visible. In those cases, ask the clinic directly about their outcomes from egg thaw cycles and embryo transfers using frozen material.
Be cautious about over-interpreting live birth per cycle
Clinics are incentivized to make their live birth per retrieval cycle look high, which can lead to some concerning practices like encouraging patients to transfer an embryo right away instead of banking multiple embryos for future family-building, or discouraging care for “poor responders” who may require multiple retrievals. These choices may boost reported rates but aren’t always in a patient’s best interest.
For intended parents hoping to have more than one child using the same donor, it may be smarter to focus on embryo banking before any transfer. But this approach - although strategic - can negatively impact the clinic’s live birth per cycle numbers. That’s why it's important to ask how your clinic approaches embryo banking and cumulative success planning.
Other questions to ask beyond the numbers
While SART data is valuable, it’s only one part of the clinic evaluation process. Consider also asking:
- What’s the average number of embryos your clinic transfers per cycle?
- How do you support intended parents using donor eggs or gestational carriers?
- What’s the experience like for people working with donor eggs?
You might also want to explore patient reviews on sites like FertilityIQ or attend a clinic info session to get a better feel for their values and communication style.
Bottom line
SART data can be a powerful tool when selecting a fertility clinic if you know how to use it wisely. Focus on donor egg cycles, apply relevant filters, and pay close attention to metrics like number of transfers, singleton birth rate, and outcomes per embryo transfer. Use the data to inform your questions, not as the only measure of quality.
Look for transparency, clarity, and a clinic that welcomes your questions. The right data can support your decision, but trust and care matter just as much.
If you work with Cofertility, we can help connect you with one of our many clinic partners.
Read more:

Choosing an Egg Donor: The Role of Biomarkers
Choosing the right egg donor involves more than just age. Learn how fertility doctors use AMH, AFC, and age together to predict egg yield and guide your family-building decisions.
If you're pursuing egg donation to build your family, you’ve probably heard that age matters. However, when it comes to the number of eggs a donor might produce in a single cycle, age is only part of the picture. Fertility doctors use a combination of biological indicators called ovarian reserve markers to get a clearer sense of how a donor is likely to respond to stimulation medication. These markers include AMH (anti-Müllerian hormone), AFC (antral follicle count), and yes, age. Together, they can help predict how many eggs a donor might yield in a given cycle.
Understanding these biomarkers can help you make better decisions: whether that’s about which donor to match with, whether to split a cohort, or whether you may need multiple cycles to meet your family-building goals. This article explains what each of these markers means, how they’re used in donor screening, and what they can (and can’t) tell you about potential outcomes.
Donor AMH: anti-Müllerian hormone
AMH is a hormone released by cells in developing egg follicles. It gives a general sense of a person’s’s ovarian reserve, or the number of eggs they still have. In most people, AMH levels peak in the mid-20s. For intended parents working with an egg donor, a higher AMH level usually suggests the donor has a good chance of responding well to ovarian stimulation, meaning more eggs are retrieved in a single cycle.
That said, there’s a wide range of what’s considered “normal,” and AMH is just one piece of the puzzle. A very high AMH might raise the risk of ovarian hyperstimulation syndrome (OHSS), especially in donors with polycystic ovary syndrome (PCOS). While high AMH may seem appealing at first glance, it still needs to be considered within the broader clinical context. On the other hand, a lower AMH doesn’t necessarily mean a donor isn’t a good candidate, especially if they’re young and have a good antral follicle count.
At Cofertility, an AMH level of at least 2.0 ng/mL is required for our donors. This threshold is based on clinical data suggesting that donors with this level are more likely to have a strong response to fertility medications and produce enough eggs to support both donation and personal use.
AMH is measured through a simple blood test and is often one of the first screening tools used to assess a donor’s fertility potential.
Read more in Does AMH Matter When Choosing an Egg Donor?
Donor AFC: antral follicle count
Antral follicle count is a snapshot of how many follicles are visible on a donor’s ovaries at a particular point in their cycle, usually early in the menstrual cycle, when baseline testing is done. These are the small, fluid-filled sacs that each contain an immature egg. During a stimulation cycle, the follicles grow larger and the eggs inside them mature ,making them available for retrieval.
AFC is measured by transvaginal ultrasound, and it gives a real-time look at the ovaries. The more antral follicles, the higher the potential number of eggs that could be retrieved. In clinical terms, a “normal” AFC is typically somewhere between 10 and 20 follicles (counting both ovaries), but many donors exceed that.
AFC is considered one of the most reliable indicators of ovarian response. While AMH tells you about the pool of follicles available in a more general sense, AFC shows you what’s happening right now. Since AFC is a real-time snapshot of the ovaries, it can fluctuate slightly from month to month, but these variations are typically minor and don’t significantly impact how a donor is expected to respond. For intended parents, a donor with a strong AFC may provide reassurance that the stimulation cycle will likely yield a solid number of mature eggs.
Donor age: still an important piece of the puzzle
You already know age is a factor. But what’s important to understand is that age affects not just the number of eggs a donor may produce, but also the quality of those eggs—specifically, their likelihood of leading to a healthy embryo.
That’s why most egg donation programs set an age range for donors, usually between 21 and 33 years old (we follow these guidelines at Cofertility). While there’s no legal maximum age to become an egg donor, the American Society for Reproductive Medicine (ASRM) recommends that donors be under 34, and most clinics follow that guidance. Our limit accounts for the fact that it can take some time to match with intended parents and complete a cycle, and we want donors to still fall within the recommended age window by the time the cycle takes place.
Within that range, there can still be differences in both quantity and quality of eggs based on things beyond age.
That said, most donors who get medical clearance respond very well to stimulation and produce excellent-quality eggs, whether in their late 20s and early 30s. Age is just one variable, and when combined with the other biomarkers, it helps doctors build a fuller picture of what to expect from a cycle.
How these markers are used together
No single biomarker tells the whole story. Fertility doctors look at AMH, AFC, and age together to estimate a donor’s likely response to ovarian stimulation. This is sometimes called “ovarian reserve testing,” but the goal isn’t just to count eggs. It’s also to plan appropriately for stimulation protocols and optimize outcomes.
For example, if a donor has high AMH and high AFC, they might be expected to produce 20+ eggs in a cycle, and the care team may start with a lower dose of stimulation medications to reduce the risk of overstimulation. If another donor has AMH on the lower end of the normal range and an average AFC, the team may anticipate a more moderate yield (perhaps 10 to 15 eggs) and plan accordingly by using a higher starting dose of medications to optimize their response to treatment.
Limits of prediction
While AMH and AFC are helpful, they’re not crystal balls. A donor with stellar biomarkers could still have a retrieval cycle that yields fewer mature eggs than expected. Likewise, a donor with average numbers might surprise everyone with a strong response.
Biology isn’t always predictable, and cycle outcomes can vary even in the same donor across multiple cycles. That’s why experienced clinics combine biomarker data with close monitoring during the stimulation phase to make adjustments in real time.
It’s also worth noting that the number of eggs retrieved isn’t the only metric that matters. Fertilization rate, embryo development, and success rates with IVF transfer all depend on additional factors,some of which can’t be measured ahead of time.
What this means for you as an intended parent
As you look through donor profiles, you may see some numbers directly—such as AMH or age—or you might get a broader summary from your clinic about the donor’s reproductive potential. It’s a good idea to ask your doctor what these biomarkers might suggest about how many eggs the donor is likely to produce, and how that aligns with your goals.
That said, it’s important to understand that every donor listed has already cleared a rigorous screening process. Fewer than 5% of applicants are accepted into Cofertility’s egg sharing program. If a donor has made it through, it means our medical advisors (who are board-certified reproductive endocrinologists) have reviewed their health, biomarkers, and ovarian reserve, and determined if they’re likely to respond well to treatment.
Within this highly qualified group, small differences in biomarker levels may not translate to big differences in actual outcomes. Rather than fixating on a slightly higher AMH or AFC, it may be more helpful to focus on which donor feels like the right match for your family, whether that’s based on their background, values, personality, or something less tangible that just clicks for you.
The bottom line
AMH, AFC, and age can offer helpful insight into how many eggs a donor may produce and how your doctor will approach their care during the cycle. These biomarkers are useful tools for setting expectations and guiding decisions, but they’re not guarantees.
All egg donation involves some level of uncertainty, even with strong indicators. That’s why programs like Cofertility set high standards up front. This ensures that every donor in the pool has a solid chance of success. Once a donor is approved, the differences between candidates tend to narrow, and the best choice is often the one that feels most aligned with your values and goals—not just the numbers.
Ask questions, gather information, and talk with your care team. But don’t be afraid to trust your gut, too. The right match will meet both the medical criteria and feel like someone who could help you build the family you’ve been hoping for.
Read more:
- Why Egg Donor Age Matters (And Why It Doesn't)
- Does AMH Matter When Choosing an Egg Donor?
- Will My Baby Look Like Me If I Use an Egg Donor?
- Shared vs. Separate Egg Donor Cycles: A Guide for Gay Dads
