fertility clinics

How to Use SART Data to Evaluate Fertility Clinics for Donor Egg IVF
Wondering how to evaluate fertility clinics for donor egg IVF? The SART database is a helpful place to start—but only if you know how to read between the lines. Here’s what to look for (and what to question).
When you’re pursuing egg donation to build your family, choosing the right fertility clinic can feel overwhelming. Everyone wants the best outcomes possible and while there’s no perfect formula for picking a clinic, the Society for Assisted Reproductive Technology (SART) database is one tool we have to evaluate IVF clinics.
SART collects detailed outcome data from hundreds of clinics across the U.S., reporting on everything from the number of cycles completed to live birth rates by patient age and treatment type. But understanding what the numbers mean and how to apply them to your unique family-building plans takes a bit of interpretation. For example, a clinic that reports higher live birth rates might simply be selecting patients with fewer fertility barriers, while another with more modest numbers could be working with harder-to-treat cases, including people with diminished ovarian reserve or complex medical histories.
This article walks through how to make sense of the SART Clinic Report, what success rates do (and don’t) tell you, and which filters are most relevant when you’re planning to use donor eggs. We’ll also cover red flags to watch for and other questions you should be asking alongside the data.
What SART data can tell you—and what it can’t
SART data is one of the most widely used sources for clinic success rates, as it reflects real outcomes, including pregnancies and live births after IVF. But it’s not a perfect apples-to-apples comparison tool. For starters, SART data is self-reported by clinics and reviewed for consistency, but not independently audited in full.
SART data also lags about two years behind, since it only includes cycles that have had time to result in a live birth. If you’re working with a newer clinic, they could be tracking and reporting outcomes to SART but just may not be reflected in the dataset quite yet.
The data is reported by cycle start, which includes any patient who initiated an IVF cycle, even if they didn’t proceed to egg retrieval or embryo transfer. That means reported live birth rates may include a denominator of patients who never got far enough for the treatment to have a real chance of success. Some clinics work hard to include every patient in their reported data; others may be more selective about who they treat, which can make their success rates appear higher.
Still, if you understand what you’re looking at, SART data can provide real insight, especially when you use filters and hone in on metrics that apply to your situation.
Looking up donor egg cycles in the SART report
To start, you can look up an IVF clinic by name or location here. If a clinic has multiple locations: they may have profiles associated with every location or they may only have profiles associated with their primary labs. The search functionality is also a bit sensitive; if you’re not locating a clinic by name, try searching by city or state.
When viewing a clinic’s report, you’ll see multiple sections, each focusing on different treatment types: cycles using a patient’s own eggs, cycles using donor eggs, and cycles using donated embryos. For intended parents working with an egg donor and possibly a gestational carrier, the donor egg data is most relevant.
Here’s what you’ll see in the donor egg section:
- Fresh donor egg cycles: These are cycles that involve using fresh donor eggs and a fresh embryo transfer.
- Frozen donor egg cycles: These are cycles that involve using frozen donor eggs and a fresh embryo transfer.
- Donor egg thawed embryos: These are cycles using frozen embryos (thawed before transfer) that were made with either fresh or frozen donor eggs.
- Donated embryos: These involve embryo transfers using embryos that were originally created by another individual or couple. These are all frozen embryo transfers.
Each of these comes with its own success rates, reported by age and often by the number of embryos transferred.
Understand the difference between a Fresh vs Frozen Embryo Transfer.
How to interpret success rates in the SART report
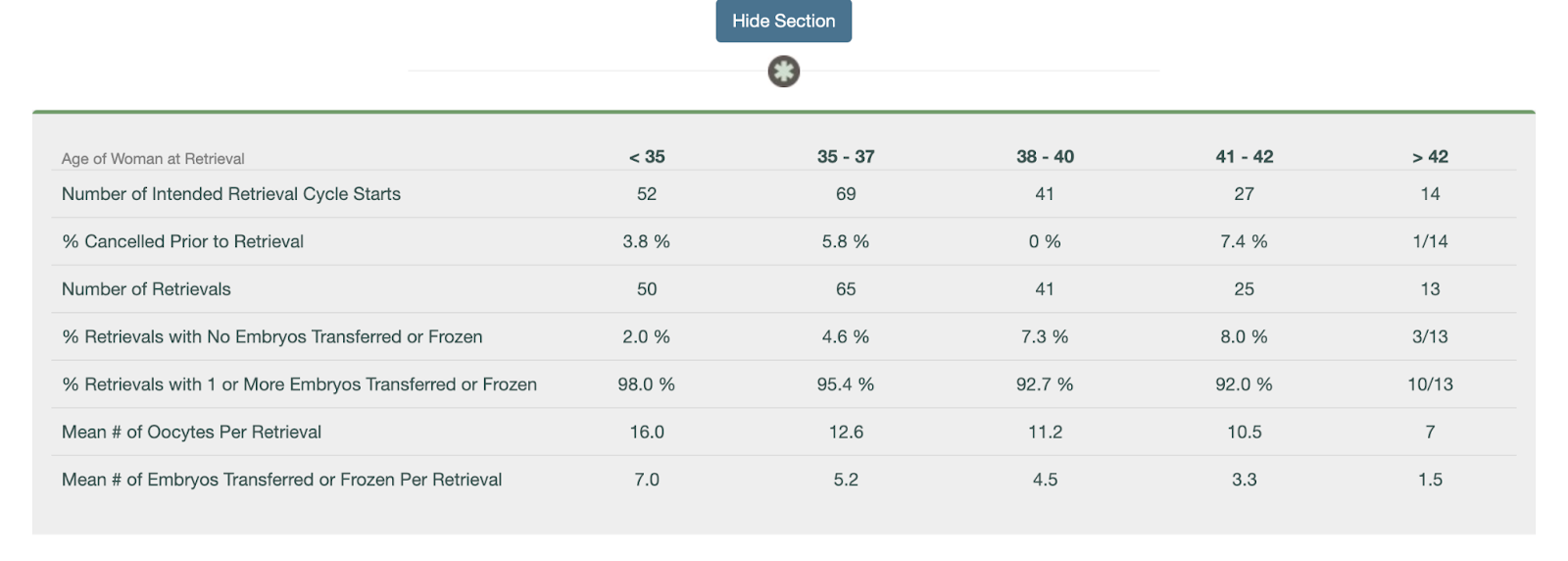
Once you’ve identified the donor egg section of a clinic’s SART report, you can start digging into the numbers. While the report doesn’t include every metric (like implantation rate), it does offer helpful data points to understand how often donor egg cycles result in live births—and how experienced the clinic is with this kind of care.
Here’s how to use the data:
- Look at the total number of embryo transfer procedures. This tells you how many donor egg transfers the clinic performed, which can give you a sense of their experience. A higher number means the clinic is regularly working with donor egg IVF families—an important signal if you’re pursuing this type of treatment.
- Check how many of those transfers resulted in live births. If there are fewer than 10 cycle starts in a category, live births are provided as a fraction. If there are 11 or more cycles, it’s provided as a percentage. While this isn’t a perfect metric, it offers a practical look at how effective the clinic is once a transfer occurs.
- Review singleton vs. multiple birth rates. A high singleton rate suggests the clinic emphasizes single embryo transfer (eSET), which is generally safer for both the carrier and the baby. High twin rates may boost reported pregnancy success but come with higher medical risks.
- If you’re using a gestational carrier (GC), ask the clinic for donor egg + GC outcomes. SART doesn’t break this out, but clinics should be able to provide this data. These cycles tend to be highly optimized and can reflect the clinic’s best-case outcomes.
While the SART report doesn’t show everything, it provides a meaningful snapshot of how well a clinic performs with donor egg cycles and how often they’re managing them. Combine this data with direct questions to the clinic to get a fuller picture of what you can expect.
Consider volume, but don’t assume more is always better
SART data shows how many cycles a clinic performs in a given year. Higher volume can indicate more experience and familiarity with a wide range of cases, but that doesn’t mean bigger is always better. A massive clinic might have shorter visit times, less personalized attention, or limited communication with physicians. Conversely, smaller clinics may offer more personalized care but might not have the same technological resources or lab investment.
Ask yourself what matters more to you: personalized attention and consistency, or access to a busy, highly specialized team? There’s no right answer—just what fits your preferences.
Don’t ignore what’s missing
Some clinics don’t report data to SART at all. While SART participation is voluntary, transparency should be a baseline expectation. If a clinic doesn’t report, ask why. It might be a red flag, or it might be an early-stage clinic without a full year of data yet.
It’s also worth noting that SART doesn’t report standalone success rates for thawed eggs (only fresh embryo transfers). So if you’re using frozen donor eggs—or if you’re planning to freeze embryos now and transfer later—those specific success rates won’t be visible. In those cases, ask the clinic directly about their outcomes from egg thaw cycles and embryo transfers using frozen material.
Be cautious about over-interpreting live birth per cycle
Clinics are incentivized to make their live birth per retrieval cycle look high, which can lead to some concerning practices like encouraging patients to transfer an embryo right away instead of banking multiple embryos for future family-building, or discouraging care for “poor responders” who may require multiple retrievals. These choices may boost reported rates but aren’t always in a patient’s best interest.
For intended parents hoping to have more than one child using the same donor, it may be smarter to focus on embryo banking before any transfer. But this approach - although strategic - can negatively impact the clinic’s live birth per cycle numbers. That’s why it's important to ask how your clinic approaches embryo banking and cumulative success planning.
Other questions to ask beyond the numbers
While SART data is valuable, it’s only one part of the clinic evaluation process. Consider also asking:
- What’s the average number of embryos your clinic transfers per cycle?
- How do you support intended parents using donor eggs or gestational carriers?
- What’s the experience like for people working with donor eggs?
You might also want to explore patient reviews on sites like FertilityIQ or attend a clinic info session to get a better feel for their values and communication style.
Bottom line
SART data can be a powerful tool when selecting a fertility clinic if you know how to use it wisely. Focus on donor egg cycles, apply relevant filters, and pay close attention to metrics like number of transfers, singleton birth rate, and outcomes per embryo transfer. Use the data to inform your questions, not as the only measure of quality.
Look for transparency, clarity, and a clinic that welcomes your questions. The right data can support your decision, but trust and care matter just as much.
If you work with Cofertility, we can help connect you with one of our many clinic partners.
Read more:
.png)
8 LGBTQ+ Friendly Fertility Doctors
We created this curated list of LGBTQ+ Friendly Fertility Doctors across the U.S. who not only offer third-party reproduction services, but who also have a proven track record of supporting queer families with respect, compassion, and expertise.
Finding the right fertility doctor is an important step in the family-building process, especially for LGBTQ+ individuals and couples who may face unique medical, legal, and emotional considerations. Whether you're a gay dad egg donation, a trans person preserving fertility ahead of gender-affirming care, or a lesbian couple navigating reciprocal IVF, having an affirming, knowledgeable provider makes all the difference.
That’s why we created this curated list of LGBTQ+ Friendly Fertility Doctors across the U.S. who not only offer third-party reproduction services, but who also have a proven track record of supporting queer families with respect, compassion, and expertise.
Brent Monseur, MD, ScM, FACOG (Palo Alto, California)
Dr. Monseur is a board-certified obstetrician/gynecologist and the founding director of the LGBTQ+ Family Building Clinical Research Program at Stanford University School of Medicine. They are an Instructor in the Department of OBGYN and lead a highly specialized team dedicated to improving reproductive outcomes for sexual and gender minority populations. They completed a fellowship in Reproductive Endocrinology & Infertility at Stanford University after finishing an OBGYN Residency at Thomas Jefferson University. Dr. Monseur received a medical doctorate from the Medical College of Virginia. They trained as a reproductive biologist at the Johns Hopkins Bloomberg School of Public Health where they completed a Master of Science degree. Dr. Monseur received a Bachelor of Science degree in Biochemistry with a concentration in Spanish from the University of Mary Washington.
They have received numerous awards for their work with the LGBTQ+ community including the inaugural Stanford Graduate Medical Education Award for Promoting Health Equity, the Diversity Fellowship Research Award from the American Society for Reproductive Medicine, and an NIH Health Disparities Research Loan Repayment Program award. They serve as a chair of the American Society for Reproductive Medicine’s LGBTQ+ Special Interest Group and have previously served as a board member of two non-profit organizations dedicated to reproductive justice: Medical Students for Choice and Path2Parenthood (now Family Equality).
Dr. Guy Ringler (Los Angeles, California)
Dr. Guy Ringler is board-certified in Obstetrics and Gynecology and Reproductive Endocrinology and Infertility at Pinnacle Fertility. He is a proud partner with California Fertility Partners.
An international leader in surrogacy and third-party reproduction, Dr. Ringler has helped patients from across the globe, including Europe, Asia, Australia, and Africa. He was one of the world’s first physicians to help gay men have babies through egg donation and surrogacy. He is committed to helping all members of the LGBTQ community fulfill their dreams of having children and building families.
Dr. Jaun Alvarez (Chicago, Illinois)
Dr. Juan Alvarez is a double board-certified Reproductive Endocrinologist and Infertility Specialist (REI) at KindBody in Chicago. He received his medical degree from the University of Illinois College of Medicine in Chicago and completed his fellowship training in Reproductive Endocrinology and Infertility at UCLA Cedars-Sinai in Los Angeles. Prior to his fellowship, he completed his Ob/Gyn residency at Emory University School of Medicine in Atlanta, GA.
He is passionate about all aspects of infertility treatment but has a particular interest in third-party reproduction, fertility preservation, diminished ovarian reserve and how obesity impacts fertility, a topic which he researched extensively during his fellowship. As a member of the LGBTQ+ community and fertility specialist, he has a special interest in LGBTQ+ fertility care and education.
Samantha Estevez, MD (Pittsburgh, Pennsylvania)
Dr. Estevez specializes in reproductive endocrinology and infertility and is board-certified by the American Board of Obstetrics and Gynecology. She practices at UPMC Magee-Womens Center for Fertility and Reproductive Endocrinology and UPMC Center for Fertility & Reproductive Endocrinology and is affiliated with UPMC Magee-Womens Hospital and UPMC Altoona. Dr. Estevez received her medical degree from Northwestern University Feinberg School of Medicine and completed her residency at Hofstra/Northwell Zucker School of Medicine, followed by a fellowship at Icahn School of Medicine at Mount Sinai. Dr. Estevez has completed training on how to create a safe, comfortable, and welcoming environment for LGBTQIA+ patients.
Dr. Allison Bloom (Bryn Mawr, Pennsylvania)
Allison Bloom, DO, MPH is a specialist in reproductive endocrinology and infertility and directs Main Line Fertility’s Third Party and Egg Donor programs. Dr. Bloom also serves as the Global LGBTQ+ Ambassador for The Prelude Network. She joined MLF as a fellow in 2017 and began practicing as an attending physician in 2020. In the five years prior to fellowship, Dr. Bloom practiced Obstetrics and Gynecology at Pennsylvania Hospital.
Dr. Bloom is experienced in the field of in vitro fertilization with a particular interest in recurrent pregnancy loss, polycystic ovarian syndrome, egg freezing, and LGBTQ+ family building. In addition to her medical training, Dr. Bloom earned a Masters in Public Health and is an advocate for fertility awareness and education. She truly believes in teaching and empowering her patients. Dr. Bloom and her wife underwent infertility treatment for over a year before successfully conceiving with IVF and welcoming twin boys into their family.
Dr. Julian Escobar (Dallas, Texas)
Dr. Julian Escobar is board certified in both Reproductive Endocrinology & Infertility and Obstetrics & Gynecology at Concieve Fertility Center. After attending high school in the DFW, he graduated with high honors in Genetics from the University of Georgia and was subsequently awarded prestigious research fellowships at the National Institutes of Health and Harvard Medical School. He then obtained his medical degree from the University of Pittsburgh School of Medicine and completed his OBGYN residency at Northwestern University in Chicago. He later relocated back to Dallas to pursue fellowship training in Reproductive Endocrinology and Infertility at UT Southwestern Medical Center.
Daniel A. Skora, M.D. (Dallas, Texas)
A member of the LGBT community himself, Daniel A. Skora, M.D., is a physician at Fertility Specialists of Texas and serves as medical director of third-party and LGBTQ+ services. He is board-certified in both Obstetrics and Gynecology, and Reproductive Endocrinology and Infertility. Dr. Skora graduated cum laude with his Bachelor of Arts degree in psychology with a certificate in neuroscience from Princeton University. He received his medical degree from the University of Minnesota Medical School.
Dr. Skora completed his residency at George Washington University Hospital and his fellowship at The Larner College of Medicine at the University of Vermont. Dr. Skora is passionate about all aspects of infertility. He is dedicated to addressing the unique needs of the whole patient and calls upon his education and experience in psychology to help each one overcome the emotional challenges of trying to conceive. Dr. Skora is a member of the American College of Obstetrics and Gynecology. He lives in Dallas, Texas with his husband, loves to travel (se habla Espanol) and spoils his two nephews whenever possible.
Austin Johnson, MD, FACOG (Seattle, Washington)
Dr. Johnson is a board-certified OB-GYN and current clinical fellow in Reproductive Endocrinology and Infertility at UW Medicine. Dr. Johnson believes in equitable access to family-building options and treatments for all individuals. He understands that the journey to building a family can be difficult for many. He, therefore, strives to help his patients reach their family-building goals by providing evidence-based care and treatment options.
Dr. Johnson's clinical expertise includes LGBTQI+ family building, fertility preservation options for transgender and oncology patients, infertility treatments, in vitro fertilization (IVF), intrauterine insemination (IUI), egg/embryo freezing, hysteroscopy, laparoscopic/robotic surgery, fibroid management, ovulation disorders, reproductive endocrinologic disorders, uterine anomalies, and endometriosis.
━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━━
We know that building your family as an LGBTQ+ person can come with added layers of complexity—but you shouldn’t have to navigate it alone. Our team is here to help you on this journey.
And if you know of a provider who belongs on this list, we’d love to hear from you. Email us at hello@cofertility.com so we can continue growing this resource for our community.
You deserve providers who see you, support you, and celebrate every path to parenthood. 💜
.png)
What is Third-Party Reproduction (TPR)?
In this article, dive into TPR, exploring its various facets, the science behind it, and the unique considerations involved. Whether you're a couple struggling with infertility, a single parent by choice, or an LGBTQ+ individual seeking to build a family, understanding TPR can empower you to make informed decisions about your fertility journey.
As a reproductive endocrinologist (aka a fertility doctor), every day I witness firsthand the profound yearning to build a family. For many individuals and couples, the path to parenthood may not be a straightforward one. Fortunately, advancements in assisted reproductive technologies (ART) have opened doors to alternative family-building options. Third-party reproduction (TPR) can offer hope for those facing fertility challenges or seeking alternative means to complete their families. But what is it?
In this article, I'll dive into the world of TPR, exploring its various facets, the science behind it, and the unique considerations involved. Whether you're a couple struggling with infertility, a single parent by choice, or an LGBTQ+ individual seeking to build a family, understanding TPR can empower you to make informed decisions about your fertility journey.
What is third-party reproduction?
When you hear the term third-party reproduction, it’s referring to a range of techniques that involve using genetic material or gestational services from a third party, someone who is not the intended parent, to achieve pregnancy. This broadens the possibilities for those who may not be able to conceive using their own gametes (eggs and sperm) or carry a pregnancy themselves. Here's a breakdown of the types of TPR:
- Sperm donation: Viable sperm from a carefully screened donor is used to fertilize eggs through intrauterine insemination (IUI) or in vitro fertilization (IVF).
- Egg donation: Donor eggs, retrieved from a healthy egg donor who has undergone rigorous medical and psychological evaluation, are fertilized with the intended father's sperm or donor sperm for implantation in the uterus via IVF.
- Embryo donation: Frozen embryos created by another family undergoing IVF are donated to another couple or individual for implantation.
- Gestational surrogacy: A gestational carrier, also known as a surrogate, carries a pregnancy for the intended parents using an embryo created either through the intended parents' own gametes or donated sperm and eggs. The gestational carrier has no genetic link to the baby.
- Double donor: Both donor sperm and donor egg come together in IVF.
More and more families are turning to third-party reproduction to build their families. Third-party reproduction is part science and medicine, and part generosity from someone else who wants to help you build your family. There is a lot of coordination and legal work involved to protect all parties, and if you work with a group like Cofertility, we will help you all along the way.
What types of families use third-party reproduction?
Third-party reproduction (TPR) opens doors for a diverse range of individuals and couples who may not be able to conceive unassisted or carry a pregnancy to term. I have worked with so many different types of families, who come to me for various reasons. Here's a closer look at some of the families who find hope and fulfillment through TPR:
- Couples facing infertility: Infertility, the inability to conceive after one year of unprotected intercourse, affects millions of couples worldwide. TPR can offer hope for those struggling with infertility due to various factors including low sperm count, blocked fallopian tubes, or hormonal imbalances. For these couples, TPR, whether through sperm donation, egg donation, or even embryo donation, allows them to experience the joy of parenthood and build their families.
- Single parents by choice: An increasing number of single intended parents are opting for TPR to build their families. They can utilize sperm donation, egg donation, and/or surrogacy to create their dream families.
- LGBTQ+ families: TPR plays a significant role in expanding family-building options for LGBTQ+ individuals and couples. Same-sex male couples can utilize egg donation and surrogacy to have a biological child within their family. Lesbian couples have the option of using sperm donation, either from a known or anonymous donor, and either partner can carry the pregnancy or utilize a gestational carrier. Transgender individuals can also explore TPR options to complete their families.
- Individuals with medical conditions: Certain medical conditions may render pregnancy unsafe or even impossible. Uterine fibroids, endometriosis, or a history of complex medical procedures or births are just some examples. TPR, through gestational surrogacy, allows these women to experience parenthood by having a genetically related child (through egg donation and sperm from their partner) or by adopting an embryo.
- People with genetic concerns: For couples at risk of passing on a known genetic condition to their biological children, TPR offers a path toward a healthy family. Preimplantation genetic diagnosis (PGD) can be performed on embryos created through IVF, allowing for the selection of embryos free from the identified genetic condition. This can give couples peace of mind and increase their chances of having a healthy child.
Regardless of the specific route taken through TPR, the common thread is the unwavering desire to build a loving family. While genetics play a role, the emotional bonds cultivated through love, nurturing, and shared experiences are the true cornerstones of a family. Studies have shown that children born through TPR thrive in loving environments and develop strong attachments to their intended parents.
The emotional journey of TPR
The decision to pursue TPR is rarely made lightly. It's often born out of a deep longing for parenthood and may be accompanied by a spectrum of emotions. Intended parents may experience a mix of hope, excitement, anxiety, and sometimes even a sense of grief if facing infertility or the inability to use their own genetic material. Open communication is absolutely vital – between intended parents, with any known donors or gestational carrier, with your agency, and within oneself. Exploring personal feelings and expectations throughout the process is essential for ensuring everyone is emotionally aligned.
Donors and gestational carriers also carry complex emotional feelings throughout the process. Donors may derive a sense of altruism and fulfillment from helping others build families. Gestational carriers often express feelings of deep satisfaction from carrying a child for intended parents who cannot do so themselves. However, feelings of uncertainty, potential vulnerability, and even moments of hesitation are also natural parts of the experience.
Psychological support in the form of counseling provides a safe space to unpack these emotions for everyone involved. It can help intended parents cope with potential setbacks, foster healthy communication with stakeholders, and build a strong emotional foundation as they navigate their unique path to parenthood.
If you work with Cofertility, we have a fertility psychologist on our team who supports all parties involved.
Do I need a doctor who specializes in third-party reproduction?
The short answer is yes! Building a family through third-party reproduction involves a mix of medical, legal, and emotional considerations. While seeking guidance from any fertility doctor is a good starting point, partnering with a board-certified reproductive endocrinologist who specializes in TPR will go a long way. These specialists possess in-depth knowledge of the various TPR techniques, from sperm and egg donation to embryo donation and gestational surrogacy. Their expertise allows them to create tailored treatment plans that perfectly align with your unique circumstances – whether that means selecting the right donor, navigating IVF procedures, or understanding complex legal agreements.
A fertility doctor with TPR experience understands the potential risks and necessary medical monitoring throughout the process. They ensure your safety and well-being, always keeping your best interests in mind. Perhaps just as importantly, they offer compassionate support throughout your emotional journey, answering any questions and providing a safe space to process the complex feelings that may arise. Building a trusting relationship with your doctor is important when making personal decisions that affect your ability to build a family.
Finding the right specialist takes a little research. Look for board-certified reproductive endocrinologists affiliated with reputable fertility clinics that offer comprehensive TPR services. Ask for recommendations from trusted sources or schedule consultations with a few specialists to find a provider whose approach aligns with your needs. Ask them about their experience with TPR, and how they approach treatment differently. Ultimately, a specialist in TPR will be your invaluable guide, increasing your chances of a positive outcome on your path to creating the family you've always dreamed of.
Summing it up
Third-party reproduction (TPR) is a powerful testament to where science and compassion meet. It expands our horizons of possibility, offering alternative paths to parenthood for many individuals and couples. Whether it's sperm donation, egg donation, embryo donation, or working with a gestational carrier – the techniques behind TPR are ever-evolving, giving more people the chance to fulfill their dreams of family.
While the science is complex, the heart of TPR is simple: it's about love, determination, and the generosity of those who offer the incredible gift of helping others build their families. Naturally, navigating the medical, emotional, and legal aspects of TPR necessitates a guiding hand. That's where a specialized reproductive endocrinologist, a team like Cofertility, and a strong support system are invaluable, turning what can seem daunting into a well-supported, empowering journey.
If this is a path calling to you, know that you're not alone. Seek out the knowledge and support that will enable you to make informed choices and feel confident at every step along the way. The joy of parenthood, experienced through whichever means resonate with you, is a beautiful path of unwavering love.
Find an amazing egg donor at Cofertility
At Cofertility, our program is unique. After meeting with hundreds of intended parents, egg donors, and donor-conceived people, we decided on an egg donation model that we think best serves everyone involved: egg sharing.
Here’s how it works: our unique model empowers women to take control of their own reproductive health while giving you the gift of a lifetime. Our donors aren’t doing it for cash – they keep half the eggs retrieved for their own future use and donate half to your family.
We aim to be the best egg-sharing program, providing an experience that honors, respects, and uplifts everyone involved. Here’s what sets us apart:
- Human-centered. We didn’t like the status quo in egg donation. So we’re doing things differently, starting with our human-centered matching platform.
- Donor empowerment. Our model empowers donors to preserve their own fertility, while lifting you up on your own journey. It’s a win-win.
- Diversity: We’re proud of the fact that the donors on our platform are as diverse as the intended parents seeking to match with them. We work with intended parents to understand their own cultural values — including regional nuances — in hopes of finding them the perfect match.
- Embryo guarantee. We’re committed to helping your family grow, and proud to offer a generous Embryo Guarantee to every intended parent we work with.
- Lifetime support: Historically, other egg donation options have treated egg donor matching as a one-and-done experience. Beyond matching, beyond a pregnancy, beyond a birth…we believe in supporting the donor-conceived family for life. Our resources and education provide intended parents with the guidance they need to raise happy, healthy kids and celebrate their origin stories.
We are obsessed with improving the family-building journey — today or in the future — and are in an endless pursuit to make these experiences more positive. Create a free account to get started today!
Read more:
